Phantom limbs
From Psy3242
Contents |
Overview
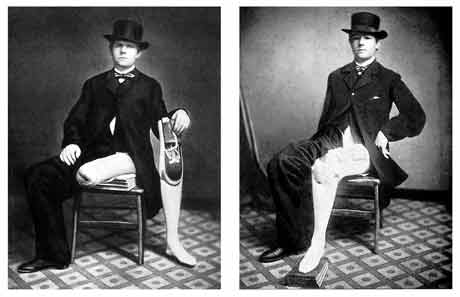
Phantom limbs is a disorder of peripersonal space, in which deficits in the spatial boundary of the visual receptive fields are observed. Most notably, it refers to a sense of outstanding and often painful feeling (98% of reported cases) from an amputated body part, such as the arms or legs, which is usually most pronounced following surgery and becomes lessened overtime (Silvano, Berger, Keith, & Brodie, 1974-1986). These sensations are not limited to pain, but also include touch, temperature, wetness, and movement that arise from the no longer existent body part (Stirling, 65). It should also be noted that this phenomenon is not metaphorical in nature, but rather a sensation that is actually felt by such individuals. In fact, the realistic nature of phantom limbs is such that a patient may actually forget that a body part has been removed and attempts to use the missing limb have been widely reported (Stirling, 66). The patient also tends to exhibit a greater conscious awareness of the phantom than the opposite, intact limb (Silvano & Reiser, 1974-1986). The three most common types of the phantom are: a mild, tingling feeling; a momentary “pins and needles” sensation; and painful feelings such as “twisting,” “burning,” “itching,” and “pulling” (Silvano & Reiser, 1974-1986).
As mentioned, most individuals experience pain that can be modified or reduced via surgical procedures, but these operations have often failed to fully eliminate such displeasure (Silvano & Reiser, 1974-1986). The ineffectiveness to diminish painful phantom limb experiences was further explored as anecdotal evidence was collected to provide insight about the underlying mechanisms of this phenomenon. Moreover, case reports have shown that stimulation of body regions aligned with the cortical receptive fields adjacent to the amputated limb can elicit the phantom experience (Stirling, 66). Vilayanur Ramachandran explained the effects of such experiences by proposing that sensory inputs travel to both target and neighboring regions and that normally, the adjacent regions are inhibited by direct inputs to the region. However, when these inputs are absent, commonly referred to as lateral disinhibition, the nearby regions now receive the cortical inputs, thereby evoking the phantom limb phenomenon (Stirling, 67). While Vilayanur Ramachandran’s assertion alone cannot account for all aspects of the experience, these findings not only highlight the need to establish methods of recovery, but they also serve as reminder that the developmental aspect of plasticity can still occur, even in mature adults (Stirling, 68).
Neural Plasticity
Vilayanur Ramachandran (1993) reported plastic changes that were observed in the visual cortex of the brain and referred to this occurrence as the “filling in” phenomenon, in which the loss of visual abilities (e.g. scotomas) caused rapid changes in the reorganization of the primary visual receptive fields. These findings led the researcher to question similar effects of other adult somatosensory pathways, including touch and hearing. Earlier studies found that after long durations of amputation, the cortical area initially corresponding to the hand was now replaced by sensory input from the ipsilateral face region. Thus, the results of these studies coupled with Ramachandran’s previous experiment generated the remapping hypothesis, which asserts the ability of the receptive fields to be temporarily expanded to proximal areas due to the “unmasking” of pre-existing neural connections, rather than the development or sprouting of new ones (Ramachandran, 1993).
Results of the study on individuals with phantom limbs, revealed a one-to-one correspondence between points on the patient’s fingers as well as on the face, which were not randomly represented, but observed on the lower face region and the area near deafferentation (Ramachandran, 1993). Additionally, it was further suggested that complex sensations distal from the region of amputation could be referred, which occur at a rapid rate of reorganization. Thus, modality-specific “rewiring” can effectively occur even after short periods of stimulus deprivation, thereby supporting Ramachandran’s hypothesis that phantom limb experience arises from spontaneous activity of tissues in the face and those near the amputated limb (Ramachandran, 1993). It was also thought that reafferance signals are combined with motor commands that are then sent to the muscle(s) of the phantom limb and to some degree, from neuromas, or tumors that are comprised of nerve tissues (Ramachandran, 1993). The information from these sources is lastly processed in the parietal cortex, which gives rise to the experience, where an image of the nonexistent body part persists. However, in response to the researcher’s own assertions, extensive studies investigating the biological, pre-existing neural connections have failed to find significant results that would support the “unmasking” hypothesis Ramachandran proposed, thereby giving greater rise to the sprouting hypothesis. If such sprouting were the case, these growths would require precise and rapid cortical reorganization to enable topography to take place as well as the occurrence of complex sensations such as “gripping,” or “trickling” (Ramachandran, 1993). While this study proved to be somewhat inconclusive in that the neither of the competing hypotheses was firmly established, the rapid changes in the topographical maps implied the need for future revision of the stable or unchanging views of cortical receptive fields.
Later, Ramachandran and Rogers-Ramachandran (2000) further explored the remapping hypothesis and indeed found that unmasking of pre-existing neural connections can be referred even hours after amputation. Similar to the results in the abovementioned study, an earlier experiment on adult monkeys revealed the topographic reorganization when a stimulus was presented to a side of the face that corresponded to the hand in the cortical somatotopic map. Following this finding, magnetoencephalographic experiments showed similar results in the adult human cortex, in that the referred feelings were modality-specific (Ramachandran & Rogers-Ramachandran, 2000). For instance, sensations that were delivered to the lower face region were also felt on the phantom limb. In addition, when other parts of the body were similarly stimulated, these sensations were not as pronounced on the phantom; however, evidence showed that a second topographical map was constructed close to the missing body part. Therefore, these results provide evidence for the remapping hypothesis, where sensations occur as a result of the unmasking of pre-existing neural connections, as shown in the rapid topographical reorganization; a finding that was previously challenged (Ramachandran & Rogers- Ramachandran, 2000).
This study also highlighted the role of the conscious experience in brain activity, in that patients initially felt sensations in both the hand and the face, apparently due to the separate activation of these two regions. However, overtime the patient would begin to experience a feeling on the just the face when the hand was touched. This gives rise to a possible “cortical overshooting” during mapping reorganization, so that sensation from the hand is suppressed or masked (Ramachandran & Rogers-Ramachandaran, 2000). Finally, the researchers reported Mirror box experiments, where a patient would place the intact body part in a location that corresponded to the represented limb. Thus, the visual illusion that the phantom limb had been resurrected provided visual feedback that enabled the troubled patient to relieve any reported displeasure that had been previously experienced (Ramachandran & Rogers-Ramachandran, 2000). The importance of these studies showed the interaction between visual and somatosensory modalities, which deal with back-and-forth exchanges, rather than the initially proposed hierarchical neural model. Furthermore, these mirror image studies implied that body image is a malleable, internal construct that is also subject to change, despite its seemingly rigid and fixed appearance (Ramachandran & Rogers-Ramachandran, 2000).
Body Image
Body image refers to the internal and actual or idealized image that manifests itself in ways that shape an individual’s personality, self-esteem, and overall psychosocial well-being. In phantom limbs patients, the cerebral representation can be reorganized, so that the phantom is modified and sometimes even dissipated. Often times though, amputation can lead to a distorted body image that is accounted for in emotional, perceptual, and psychosocial reactions (Silvano & Reiser, 1974-1986). This sudden change not only leads to a misrepresentation of the self, but also arouses varying levels of anxiety in such patients. Additionally, denial is a common defense mechanism that cannot only result in failure to report a phantom limb, but also an inability to reorganize an individual’s body image, such that recovery and rehabilitative measures cannot be effectively taken. Consequently, this maladaptation can subsequently lead to embodiment of psychopathological characteristics, which include, but not are not limited to, depression and magical thinking (Silvano & Reiser, 1974-1986). Therefore, attempts to modify the phantom limb can only be successful depending on the relational meaning of the body part to the patient. In other words, if an amputee is unwilling to accept the present body structure, as is, this perceived defect is fully capable of interfering with motivation and recovery as a result of this disturbance (Silvano & Reiser, 1974-1986). Therefore, the unstable nature of a patient’s body image should be fully accounted for in evaluation and treatment of such patients.
Treatment
Successful treatment of the disturbed body image arising from the phantom limb phenomenon is dependent upon the current body of knowledge, which unfortunately, has been inadequately implemented in the present social system (Silvano & Reiser, 1974-1986). The ways in which social life is constructed can therefore profoundly affect the self-esteem, or the manner in which a patient perceives him/herself. In cases where the social structure has failed to provide supportive measures, it is vitally crucial for rehabilitative services to appropriately develop procedures that allow for ego enhancement (Silvano & Reiser, 1974-1986). The patient should be made aware of the most commonly reported phantom experiences, and fears and desires about the amputated body part should be addressed. Family, friends, and other environmental influences should also be expected to appropriately respond to such patients, for several studies have shown the detrimental effects that phantom experiences can have on body image and consequently, personality and overall psychological structure and functioning (Silvano & Reiser, 1974-1986). Therefore, these individuals should act as support systems, upon which the patient can reliably depend.
In patients who experience chronic pain, the goal of outside resources is to adopt methods of behavioral reinforcement, or operant mechanisms, which can either, prolong or reduce the individual’s expression of pain. These strategies are referred to as Fordyce’s basic principles of behavior modification (Silvano et al., 1974-1986). The approach here is to alter the patient’s behavior such that he/she can focus on engagement in other areas that enable him/her to withdraw from the reported chronic pain and exert more effortful control over these undesirable experiences. While the aforementioned suggestions regarding this phenomenon have been widely reported, the primary emphasis should remain on the reactions of amputated patients to ensure maximum recovery and restoration of a healthy body image (Silvano et al., 1974-1986).
In similar cases of chronic pain, other forms of therapy can be taken. For instance, Sympathetic Blockade refers to the intravenous infusion of guanethidine by closing off circulation. Shortly after, the patient tends to feel less pain that can sometimes result in complete recovery, but should be repeated to guarantee permanent relief (Silvano et al., 1974-1986). Other approaches to these seemingly endless periods of pain include surgical sympathectomy and chemical sympathectomy, in which destruction of the nerves in the sympathetic system can increase blood flow and reduce pain (Silvano et al., 1974-1986). Similarly, electrical stimulation, intense vibration of the stump, and injections of hypertonic saline have also shown to relieve pain, with duration of success remaining largely dependent upon the patient (Silvano et al., 1974-1986).
Finally, the above mentioned study conducted by Ramachandran and Rogers-Ramachandran (2000) confirmed the temporary, and in some cases permanent, elimination of pain in phantom limbs patients in Mirror box experiments. As previously noted, the ability to project an individual’s intact limb to a corresponding location on the mirror creates the visual illusion of the reported phantom. This visual feedback, in turn, provides these patients with the ability to relieve unwanted sensations (e.g. clenching) pertaining to the non-existent body part (Ramachandran & Rogers-Ramachandran, 2000). However, Mirror box experiments are susceptible to “placebo effects” in relation to reduction of pain, and so it is evident that studies of double-blind control subjects should be conducted. Nonetheless, whether or not this procedure produces favorable outcomes, it should still be noted that the use of visual feedback enables patients to not only see, but also feel corresponding movements in the reported phantom, which therefore gives rise to the conscious experience of this phenomenon (Ramachandran & Rogers-Ramachandran, 2000). Disturbances in an individual’s body-image and/or experience of chronic pain have been largely observed in such patients; however, the extent to which these reactions are reported provide profound implications for which therapy methods will produce the most effective results (Silvano & Reiser, 1974-1986).
References
Ramachandran, V. S. (1993). Behavioral and magnetoencephalographic correlates of plasticity in the adult human brain. Proc. Natl. Acad. Sci. USA, 90, 10413-10420.
Ramachandran, V. S., & Rogers-Ramachandran, D. (2000). Phantom limbs and neural plasticity. Archives of Neurology, 57, 317-320.
Silvano, A., & Reiser, M. F. (Eds.). (1974-1986). American handbook of psychiatry: Organic disorders and psychosomatic medicine (2nd ed., Vols. 1-8). New York, NY: Basic Books, Inc., Publishers.
Silvano, A., Berger, P. A., Keith, H., & Brodie, H. (Eds.). (1974-1986). American handbook of psychiatry: Biological psychiatry (2nd ed., Vols. 1-8). New York, NY: Basic Books, Inc., Publishers.
Stirling, J. (2002). Introducing Neuropsychology. New York, NY: Psychology Press.