Sexual differentiation, HPG axis
From Iusmphysiology
- started here on 04/04/11.
[edit] Sexual differentiation and the HPG Axis
[edit] Learning objectives
- Prof will take exam questions from objectives.
[edit] Sexual differentiation
- Genetics is determined at fertilization.
- XY = male
- XX = female
- The sperm has either an X or a Y and donates it to the X-containing ovum.
- There are many levels of sexual differentiation:
- establishing the genetic sex
- differentiation of the gonads
- differentiation of the internal reproductive organs
- differentiation of the external genitalia
- gender role
- gender identity
[edit] Differentiation of the gonads
- As an embryo develops, the gonads become the source of gender hormones:
- In males, the gonads become the testes and provide testosterone and dihydrotestosterone.
- In females, the gonads become the ovaries and provide estrogen.
- The gonads take their developmental cues from their genotype as to how it should develop and what hormones it should produce.
- An XY gonad has a Y chromosome with the Sex-determining region Y (SRY).
- SRY is also called testis determining factor (TDF).
- SRY is the master switch that causes differentiation to head toward male.
- SRY encodes a transcription factor that is part of the high mobility group (HMG) family.
[edit] SRY and PAR on the Y chromosome
- The PAR (psudoautosomal region) of the Y chromosome is a well conserved area that allows the Y chromosome to pair with the X chromosome for cell division.
- PAR is at the very distal area of the short arm of the Y chromosome.
- SRY is located just proximal to the PAR and is considered part of the sex determining region.
- Two diseases are associated with SRY:
- SRY defects lead to XY females; Swyer syndrome.
- Translocation of the SRY region from the Y chromosome to the X chromosome yields XX males; XX male syndrome.
[edit] Differentiation of the internal genital ducts
- Initially, embryos initially have a set of undifferentiated gonads and both Wolffian ducts and Mullerian ducts.
- The ducts become the transporters of sperm or egg.
- Wolffian ducts mature into the epididymis and vas deferens.
- Mullerian ducts mature into the oviduct, uterus, and upper part of the vagina.
- Based on the genotype of the gonads (that is, the presence or absence of SRY), the gonads will begin to express hormones.
- Testes produce AMH (anti-Mullerian hormone), testosterone, and dht (dihydrotestosterone).
- AMH causes involution of the Mullerian ducts and testosterone causes proliferation of the Wolffian ducts.
- Ovaries produce no hormones embryonically.
- A lack of hormones allows Wolffian ducts to involute and causes Mullerian ducts to proliferate.
- Testes produce AMH (anti-Mullerian hormone), testosterone, and dht (dihydrotestosterone).
- The presence of hormones from the gonads determines the differentiation of the internal genitalia.
- If SRY is present:
- AMH, test, and testosterone are produced by the developing gonads
- Anti-Mullerian hormone (AMH) is responsible for degeneration of the female-associated Mullerian ducts in males
- We say that the Mullerian ducts involute; involute: "rolled inwards spirally" per [www.biology.lsu.edu/heydrjay/ThomasSay/terms.html LSU Biology]
- Gonads differentiate into testes.
- If SRY is not present:
- No hormones are produced by the developing gonads
- The Wolffian ducts atrophy.
- Gonads differentiate into ovaries.
- Note that female seems to be the default gender.
[edit] Swyer syndrome
- Recall that Swyer syndrome results from a SRY defect in an XY patient.
- Swyer syndrome is considered a type of hypogonadism because the expected male gonads did not develop.
- Swyer syndrome is considered a "pure" gonadal dysgenesis because there is no chromosomal defect; that is, they have a normal karyotype.
- Gonads are underdeveloped and are often referred to as "streaks".
- Not that though the gonads do not develop correctly in Swyer syndrome, the internal and external genitalia do develop normally.
- Note, however, that puberty does not occur normally so external genitalia do not mature through puberty.
- Patients with Swyer syndrome are often treated with estrogen and progesterone replacement therapy.
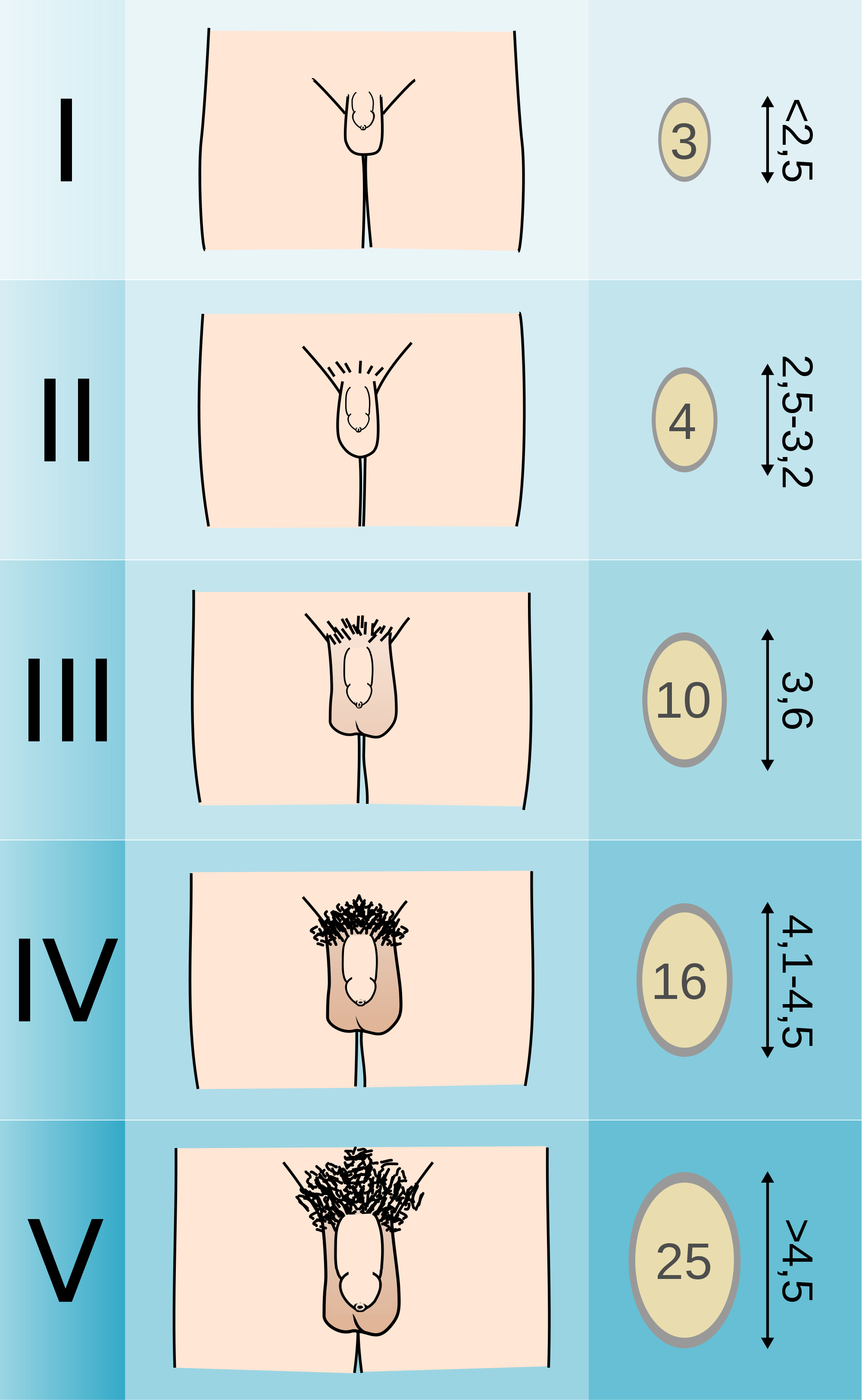
[edit] Klinefelter's syndrome
- Klinefelter's syndrome results from a 47 XXY genotype.
- XXY genotype results in poorly developed testicles.
- Underdeveloped testicles can result in non-masculine features and pro-feminine features:
- Non-masculine: poor beard growth, poor chest hair growth, frontal hair growth (lack of frontal balding), small testicular size
- Pro-feminine features: narrow shoulders, wide hips, breast development, female-like pubic hair growth
- 1:1000 males has Klinefelter's syndrome
[edit] Differentiation of external genitalia
- Like gonads and ducts (internal genitalia), the external genitalia begin in a bipotent state from which they can develop into either male or female external genitalia.
- External genitalia are signaled to develop by the presence or absence of androgens--particularly DHT.
- Male external genitalia develop in the presence of DHT.
- Female external genitalia develop in the absence of DHT.
Listen for how much anatomy we need to know.
- Said he won't ask specific details; just wants us to know that the pre-anatomy has bipotential.
- One exam question from everything previous to this comment.
[edit] Gender role
- Gender role is the gender presented by an individual to society.
- Can be independent from anatomy and chromosomes.
- Gender role can be expressed through name, clothing, physical appearance, family role, occupation, and behavior.
No exam questions on this.
[edit] Gender identity
- Gender identity is the internal conviction of one's own gender.
- We do not currently understand all the factors and complexity of gender identity.
- There is an interesting, intimate relationship between nature and nurture as it relates to development of role identity.
- Think prenatal androgen exposure, family beliefs, appearance of the genitalia, and medical / surgical experiences.
No exam questions on this.
- One exam question from everything after this comment.
[edit] Key concepts of the HPG axis
- The HPG axis is the hypothalamus-(anterior)pituitary-gonad axis.
- Note that the HPG axis also includes some activity from the cortical regions of the brain (the higher-function centers of the brain).
- Some examples of higher brain centers that affect the hypothalamus are the visual, olfactory, pineal and stress centers.
- The hypothalamus contributes to the HPG axis by releasing GnRH.
- GnRH binds to receptors on the gonadotropes of the anterior pituitary.
- The gonadotropes of the anterior pituitary contribute to the HPG axis by releasing leutinizing hormone (LH) and follicle stimulating hormone (FSH).
- The gonads contribute to the HPG axis by secreting sex steroids and peptide hormones.
- The gonads also release inhibin which feeds back on the anterior pituitary to reduce LH and FSH release.
- The gonads are also the site of germ cell production and maturation.
- Testosterone and estrogen from the gonads feed back on the anterior pituitary and the hypothalamus to reduce LH / FSH and GnRH release, respectively.

[edit] HPG axis in males
- In males, the hypothalamus releases GnRH to affect gonadotropes of the anterior pituitary.
- Upon GnRH signaling, gonadotropes of the anterior pituitary release LH and FSH to affect the testicles.
- LH and FSH negatively feedback on the hypothalamus, too.
- Upon LH / FSH signaling, the leydig and sertoli cells of the testicles release testosterone and inhibin.
- Testosterone triggers spermatogenesis and negatively feeds back on the anterior pit and hypothalamus.
- Inhibin inhibits the anterior pituitary.
- Note that testosterone is bound by ABP (androgen binding protein) in the blood.
http://www.uptodate.com/contents/images/ENDO/5463/HPG_axis_PI.jpg?title=HPG+axis+PI
[edit] HPG axis in females
- In females, the hypothalamus releases GnRH to affect gonadotropes of the anterior pituitary.
- Upon GnRH signaling, gonadotropes of the anterior pituitary release LH and FSH to affect the ovaries.
- Note that LH / FSH don't negatively feed back on the hypothalamus like they do in the male.
- Upon LH / FSH signaling, granulosa cells of the ovaries release estradiol, progesterone, inhibin, and activin.
- Estradiol and progesterone go on to affect target cells.
- Estradiole and progesterone have opposite feedback effects on the anterior pit and hypothalamus depending on the phase: positive feedback in the follicular phase and negative feedback in the luteal phase.
- This makes sense because females need to make and mature oocytes on a cycle each month.
- Activin increases FSH production and release and systemically increases proliferation.
- Inhibin decreases FSH production and release and systemically decreases proliferation
- Estradiol and progesterone go on to affect target cells.

[edit] Higher centers
- The HPG axis is affected by stress, sight, smell, and emotion.
- These emotions can generate inhibitory or stimulatory signals.
No exam questions on this.
[edit] Neurotransmitters that affect the HPG axis
- There are LOTS of NTs that affect the HPG axis: norepinephrine, dopamine, epinephrine, acetylcholine, endorphins / opioids, neuropeptide Y, leptin, serotonin, cholecystokinin, GABA-major inhibitory NT.
[edit] Hypothalamus
- The hypothalamus releases GnRH at 70-90 minute intervals; we call this autorythmicity.
- GnRH is a chromosome 8, 10mer peptide with a very short half-life--around 3 minutes.
- The cells that secrete GnRH are neurons located in the arcuate nucleus of the medial basal hypothalamus (MBH).
[edit] Immortalized GnRH secreting neurons
What is the point of this slide?
[edit] Pituitary Gonadotropins
- FSH and LH are released by gonadotrophs of the anterior pituitary.
- FSH and LH are alpha-beta in structure; alpha is identical but beta is unique.
- This won't be tested.
- Gonadotrophs are stimulated (to release FSH and LH) and inhibited by GnRH and gonad hormones, respectively.
[edit] Hypothalamus and Pituitary anatomy
- An illustration highlighting the point that gonadotropes reside in the anterior pituitary.

[edit] Pulsatile versus continuous GnRH
- When you override the pulsatile release of GnRH by infusing lots continuously, LH / FSH drops to low levels.
- So we can see that it is important that GnRH must be released pulsatile to get normal release of LH / FSH.
[edit] Control of the onset of puberty
- Puberty: the period of transition between juvenile state and adulthood, during which secondary sex characteristics appear and fertility is acquired.
- We say that puberty occurs when the HPG axis matures, but we don't know the catalyst for puberty.
- We do know that the onset of puberty is affected by many factors, including: genetics, nutrition, body weight, skeleton maturation (affects estrogen levels), altitude.
- We suspect that psychosocial and environmental factors (like environmental estrogen exposure) also play a role in determining the onset of puberty.
[edit] Mini-puberty of infancy in males
- In males, during the first month of life, there is a period of adult-like HPG axis activation.
- That is, a period where testosterone levels are equal to those of adult males.
- The function of this mini-puberty in boys is unknown.
- There is no appreciable change in physical characteristics caused by these high levels of testosterone.
[edit] Testosterone throughout the lifespan
- Testosterone is seen during the first and second trimesters of pregnancy, primarily.
- Then test is expresed during the mini puberty and begins to ramp up again during the 10-17 years (puberty).
- Test expression remains constant through most of adult life and then begins to fade in old age.
- http://books.google.com/books?id=9gvBlktAT6YC&lpg=PA1&ots=L23cN_r6NM&dq=kaefer%20m%20Mechanisms%20manifestations%20and%20management&lr&pg=PA256#v=onepage&q=testosterone&f=false
[edit] Changes in the HPG axis during puberty
- During puberty, the HPG axis is "maturing".
- Decreased sensitivity of GnRH-releasing neurons (hypothalamus) to negative feedback (from the gonad hormones) causes an increase in pulsatile GnRH release.
- Increased sensitivity of gonadotrophs (anterior pit) to GnRH causes an increase in LH / FSH secretion.
- Increased sensitivity of gonads to LH / FSH causes increased gonadal steroid production.
- stopped here on 04/04/11.
- started here on 04/05/11.
[edit] Kisspeptin and GPR54 at the Hypothalamus
- Neurons of the hypothalamus is stimulated to release GnRH when kisspeptin binds GPR54.
- GPR54 is a 7-transmembrane protein: bind extracellular signal and then transduce the signal via the cytoplasmic tail.
- Kisspeptin is one of several peptides encoded by the Kiss-1 gene.
- When GPR54-Kisspeptin signaling is interrupted, hypogonadotropic hypogonadism results from reduced LH / FSH signaling.
[edit] Characteristics of normal puberty
- There are four aspects to a normal puberty phase.
- Sexondary sexual characteristics develop: things that are not directly related to making babies (facial hair, breast enlargement, et cetera).
- Somatic growth spurt occurs
- Fertility is acquired
- Physiological changes occur
[edit] Puberty terminology
- Adrenarche: onset of adrenal and androgen production
- Precedes puberty by 2-3 years
- Occurs around 7-8 years old
- Thelarche: onset of breast bud development
- Estrogen causes thelarche
- Greek / latin: thel- nipple, female
- Pubarche: onset of pubic hair growth
- Estrogen or testosterone causes pubarche.
- Menarche: onset of menstral flow
- Average age of menarche onset in the US is 12.8 years old
[edit] Secondary sexual development
- Gonadarche: rise in gonadal sex steroids as a result of the HPG axis re-activation (recall that it was active in pre-natal development).
- Adrenarche: rise in adrenal androgens independent of gonadal sex steroid production
- We know that estrogens and androgens cause some of the changes seen in puberty because aberrant exposure to estrogens and androgens causes aberrant changes.
[edit] Physical effects of sex steroids
- Estrogena 'and androgens cause growth acceleration, skeletal maturation, and genital changes.
- Estrogens cause breast development in both boys and girls.
- Androgens cause body hair, body odor, and also causes acne in both boys and girls.
[edit] Puberty in girls
- Age of onset between 7.5 years to 13 years; average age of onset is 10.25.
- The first sign of puberty is breast buds in 70% of cases.
- Another common first sign is pubic hair.
- A second sign of puberty usually follows within 6 months.
- The peak growing time for women usually occurs 1.3 years before menarche.
- Average growth during this growth period is 9 inches.
- Menarche usually occurs 2.25 years after the onset of puberty.
[edit] Puberty in boys
- Age of onset between 9 years to 14 years; average age of onset is 12.25.
- The first sign of puberty in boys is testicular enlargement.
- One can measure the testicular volume as an indicator of enlargement.
- The peak growing time for men is usually 2 years later than in girls.
- Boys usually gain around 11 inches during pubertal growth spurt.
[edit] Puberty comparison: boys and girls
- Boys start and end later.
- Girls start earlier and proceed more rapidly through puberty.

[edit] Abnormal puberty
- There are lots of causes of abnormal puberty--some are normal variation and some are pathological.
- Any junction of the HPG axis can be involved.
- The treatment depends on the etiology.
[edit] Precocious puberty
- Precocious puberty defined as "secondary sexual development occurring in girls before the age of 7.5 / 8 (AA, Hispanic / caucasians) or in boys before the age of 9".
- There are 3 types of precocious puberty: normal variants, central, and peripheral.
- Normal variants resulting in precocious puberty can occur by way of premature thelarch (recall that thel refers to breast in greek or latin) or premature adrenarche (adrenal or adrogen production).
- Central precocious puberty arises from defects of the HPG axis.
- Peripheral precocious puberty arises from an ectopic (non HPG) source of sex steroids.
[edit] Central precocious puberty
- Most cases of precocious puberty are central precocious puberty (having to do with the HPG axis).
- Central pp (precocious puberty) results in a normal sequence of events just at an earlier time; that is, it looks just like puberty but occurs earlier in the patient's life.
- Central pp is much more common in females.
- Central pp: females > males
- Central pp's etiology is usually idiopathic.
- CNS injuries can increase the risk for central pp. (Blows to the head, spinal injuries, etc.)
- Secondary sexual development occurs gradually.
- Somatic growth (which is a normal part of puberty) also starts early, is accelerated, and is then arrested relatively early (even for precocious puberty) and thus results in short stature.
[edit] Causes of precocious puberty
- Recall that precocious puberty is ultimately the early release of sex hormones.
- Tumors or hyperactivity of the pituitary or hypothalamus can cause early release of the sex hormones.
- 60% of pp boys have an identified brain abnormality.
- Most girls under 4 with pp have an identified brain abnormality.
- 80% of girls with pp do not have an identified brain abnormality.
- Pseudoprecocious puberty results from a tumor of the adrenal / testes / ovary that releases sex hormones.
- In pseudoprecocious puberty, the gonads do not develop early (because they are not getting the required LH / FSH signaling) but the aberrant levels of sex hormones will cause secondary sexual development.
[edit] Precocious puberty: Symptoms and diagnosis
- Male and female S&S: underarm / pubic hair growth, body odor change, acne, early growth, early arrest of growth, short stature,
- Male S&S: facial hair growth, penis lengthening, appearance becomes masculine
- Female S&S: menstruation, breast development
- Recall that one difference between true and pseudo- precocious puberty is the development or lack of development in the gonads, respectively.
- In true precocious puberty, the gonads develop because there are elevated levels of LH and FSH.
- In pseudoprecocious puberty, the gonads do not develop because there are not elevated levels of LH and FSH.
- Diagnostics include measuring blood hormone levels and taking x-rays of the hand and wrists for estimates of bone development.
- CT, MRI, and ultrasound are also used to look for adrenal / hypothalamic / pituitary tumors and development of the adrenals and gonads.
[edit] A GPR54-activating mutation
- Recall that the GPR54 receptor resides on the neurons of the hypothalamus (in the MBN) and is activated by kisspeptin.
- This research identified a mutation in the GPR54 receptor that activated the receptor and caused central precociouis puberty.
- Recall that turning on GPR54 increases GnRH which increases LH / FSH at the pit which causes development of the gonads.
- Specifically, the mutation caused a decrease in receptor desensitization such that the receptor transduced an intracellular signal for a longer period of time than a wild-type receptor.
- This decreased densensitization caused increased signaling through the GnRH releasing neurons and increases GnRH release.
- This image shows the amount of phosphorylated ERK as a measure of pathway activation.
- In the disease state, there is more phosphorylated (activated) ERK present.
[edit] Peripheral precocious puberty
- Recall that peripheral precocious puberty occurs when sexual development is induced by sex steroids that do not originate from the HPG axis.
- Peripheral precocious puberty is rare and can be heritable or not.
- The non-HPG source of steroids can be endogenous or exogenous.
- Peripheral precocious puberty often demonstrates heterogeneity:
- there is often acute onset,
- there is often linear growth acceleration that results in tall stature and advanced bone age (upon xray diagnostics on the hand and wrist),
- there are many different classes of steroids to which children can be exposed,
- the duration of exposure to steroids can be quite variable.
[edit] McCune-Albright syndrome, a form of peripheral precocious puberty
- One cause of peripheral precocious puberty has been named: McCune-Albright syndrome results from an activating mutation of a G protein expressed in endocrine tissues.
- The G protein's Gs-alpha subunit is mutated into a higher activity state causing increased cAMP.
- Elevated cAMP from an over-active G protein causes hyperfunction of endocrine tissues.
- McCune-Albright is characterized by a triad of symptoms: pp, cafe au lait, and fibrous bone dysplasia.
- Large ovarian cysts are also seen in girls.
- McCune-Albright precocious puberty is an example of a somatic mutation in a mosaic distribution.
Why is it mosaic? Because it mutates during development? Yes per wikipedia
[edit] Delayed puberty
- We consider puberty delayed if there is no female onset by 13 or male onset by 14.
- We also consider pubertal development slower than one Tanner stage per year delayed puberty.
- Delayed puberty can either be "normal variant" or pathologic.
- Normal variant delayed puberty shows similar delay in both somatic growth and sexual development and often occurs with a family history of "late bloomers".
- Pathologic delayed puberty can be congenital or acquired and may be caused by a problem at any level in the HPG axis.
[edit] Conclusion
- The HPG axis is a highly integrated system with inhibitory and stimulatory modulators.
- Though we don't know the trigger for puberty, we do know the predictable series of events that normally occur.
- There are many different etiologies for abnormal puberty, many of which affect the HPG axis.
- stopped here on 04/05/11.
