Exam 2 Physical Diagnosis Objectives
From Iusmicm
[edit] Chapter 14
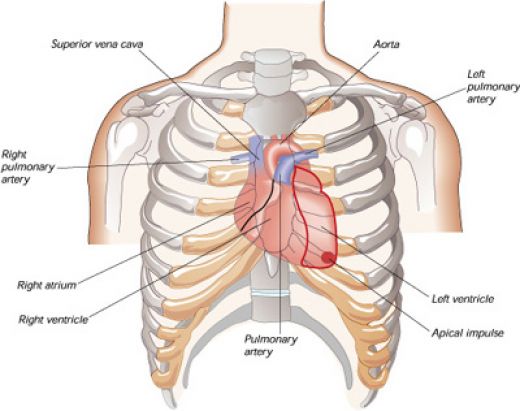
[edit] Describe and recognize the surface topography of the heart and utilize that knowledge to describe the physical findings of the heart
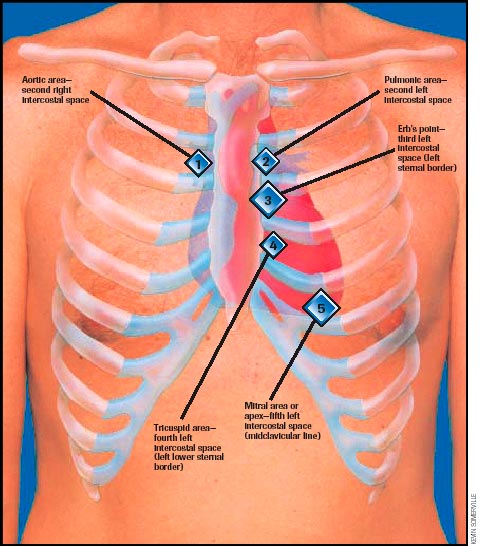
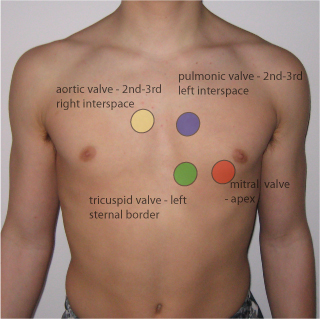
[edit] Describe and recognize the four classic auscultatory areas and Erb’s point
- The auscultation locations are focused on listening to the valves, though the names of the locations do not necessarily correlate with where the same valve is heard best.
- Aortic: second intercostal space, right sternal border (2ICS-RSB)
- Pulmonic: second intercostal space, left sternal border (2ICS-LSB)
- Tricuspid: left lower sternal border (about the fifth intercostal space; LLSB)
- Mitral: cardiac apex at the fifth intercostal space, mid-clavicular line (5ICS-MCL)
- Erb's point: third intercostal space, left sternal border (3ICS-LSB)
- Location of best pulmonic / aortic valve auscultation

[edit] Describe the cardiac cycle and be able to clinically correlate the cycle to a patient’s cardiac exam
- There are four heart sounds: S1, S2, S3, S4
- S1 is the closure of the AV valves: mitrial (left, systemic side) and tricuspid (right, pulmonary side)
- S2 is the closure of the semilunar valves: aortic (left, systemic side) and pulmonary (right, pulmonary side)
- S1 and S2 are normally audible in all individuals.
- S3 and S4 are normal in children and young adults but indicate pathology in adults.
- The presence of S3 or S4 creates a gallop sound and thus they are called gallop sounds.
- S3 occurs at the end of rapid ventricular filling.
- S3--when audible--indicates volume overload.
- Causes of volume overload may include CHF or valve lesions causing regurgitation.
- S3 has a specificity of 90%.
- NB: is is normal to hear S3 in children and youth.
- S4 occurs at the end of diastole.
- S4 can be simulated by speaking the word "middle". S4 is the "ddle" of "middle" where the "mi" is S1 (closing of AV valves).
- NB: S4 is normal in children and young adults.
- S4 in a pt older than 40 is indicative of a noncompliant or stiff ventricle.
- Pressure overload as in CHD is the cause of a noncompliant ventricle.
- Physiologic split of S2 with accompanied sinus arrythmia:
- S2 is often split, especially upon inspiration.
- During inspiration, the intrathoracic pressure is lower causing more blood from the SVC and IVC to enter the right atrium / ventricle.
- Increased right heart filling results in a longer duration of systole and therefore a later closure of the pulmonic valve.
- Thus P2 (the pulmonic component of S2--that is, the closing of the pulmonic valve) occurs later than A2 (the aortic component of S2--that is, the closing of the aortic valve).
- Initially, the return of blood from the pulmonic bed to the left heart will be relatively decreased so the left heart reflex induces sinus arrythmia.
- Sinus arrythmia is an increased heart rate after respiration and is a misnomer because it is not a true arrythmia.
- http://howmed.net/wp-content/uploads/2010/09/cardiac-cycle.bmp


[edit] Recognize the main symptoms of cardiac disease and how these symptoms can identify disease
- The main symptoms of cardiac disease are: chest pain, palpitations, dyspnea, syncope, fatigue, dependent edema, hemoptysis, and cyanosis.
[edit] Chest pain
- Not specific to the heart yet the most important.
- Angina pectoris: pain resulting from an imbalance of myocardia perfusion and myocardial functional demand.
- Classically presents as the pathognomonic Levine's sign: clutching fist over sternum with flexion at the hips.
| Descriptor | Angina | Non Angina |
|---|---|---|
| Location | Retrosternal, diffuse | Left inframammary, localized |
| Radiation | Left arm, jaw, back | Right arm |
| Character | Aching, dull, pressing, squeezing, viselike | Sharp, shooting, cutting |
| Intensity | Mild, severe | Excruciating |
| Duration | Minutes | Seconds, hours, days |
| Precipitation | Effort, emotion, eating, cold | Respiration, posture, motion |
| Relief | Rest, Nitroglycerin | Nonspecific |
- Common causes of chest pain include: CAD, aortic valvular disease, pulmonary hypertension, mitral valve prolapse, pericarditis, idopathic hypertrophic subaortic stenosis, dissection of the aorta, pulmonary embolism, penumonia, pleuritis, pneumothorax, costochondritis, arthritis, muscular spasm, bone tumor, herpes zoster, ulcer disease, bowel disease, hiatal hernia, pancreatitis, cholecystitis, anxiety, depression.
[edit] Palpitations
- Palpitations are not necessarily a sign of disease.
- Palpitations are often reported upon the occurrence of "forceful contraction" which result from increased stroke volume.
- Consider: primary cardiovascular issues, thyrotoxicosis, hypoglycemia, fever, anemia, pheochromocytoma, and anxiety.
- Consider: caffeine, tobacco, other drugs
- Common causes: atrial premature beats, nodal premature beats, ventricular premature beats, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation, multifocal atrial tachycardia, ventricular tachycardia, heart block, sinus arrest, bronchodilators, digitalis, antidepressants, smoking, caffeine, thyrotoxicosis
[edit] Dyspnea
- Paroxysmal nocturnal dyspnea occurs when the pt is supine (usually sleeping at night).
- Supine position increases blood volume in the thorax and therefore the work of the right heart, resulting in heart failure.
- Orthopnea may be reported: the need to sleep propped up on many pillows.
- Look for pitting edema in the legs as another indicator of heart failure.
- Dyspnea on exertion (DOE): occurs via pulmonary disease or chronic congestive heart failure
- Treponema: when a pt has less dyspnea when lying on the right or left side.
- General causes of dyspnea include: left ventricular failure, mitral stenosis, obstructive lung disease, asthma, restrictive lung disease, pulmonary embolism, pulmonary hypertension, anxiety, decreased oxygen pressure, and decreased oxygen carrying capacity.
[edit] Syncope
- Syncope is defined as loss of consciousness AND loss of postural tone.
- Orthostatic hypertension can lead to syncope.
- Micturition syncope occurs in older men (usually) who have to urinate during the night and (because they have just moved from supine to standing) experience syncope.
- Vasovagal syncope occurs because of a sudden fall in systemic vascular resistance without a compensatory increase in cardiac output (because of increased vagal--parasympathetic--signal).
- Usually accompanied by presyncopous s/s: pallor, nausea, weakness, blurred vision, light headedness, perspiration, yawning, diaphoresis, hyperventilation, epigastric discomfort (sinking feeling).
- Carotid sinus syncope occurs because of an hypersensitive carotid sinus (or excessive stimulation of the carotid sinus) which leads to inappropriate baroreceptor signaling that leads to hypotension and a risk of syncope.
- The reflex can cause bradycardia (slowing the heart rate, decreasing perfusion of the brain, and syncope) or vasodepression (decreased vasoconstriction, decreased perfusion, and syncope).
- Post-tussive syncope is when coughing increases the thorasic pressure (usually in pts with chronic obstructive disease) and thus activates the carotid sinus reflex and induces syncope.
[edit] Fatigue
- Most common causes of fatigue are anxiety and depression.
- Fatigue has poor specificity for cardiac issues.
[edit] Dependent Edema
- Dependent edema means that it is a function including gravity; that is, dependent edema is edema that is affected by gravity.
- Classically, dependent edema is seen in the lower limbs and it best in the morning after having been supine for hours and is worse at the end of the day when the pt has been upright and gravity has moved the fluid to the legs.
- Symmetrical swelling indicates a systemic cardio-pulmonary issue as opposed to an infectious agent.
- Cardiac causes of edema are usually preceded by dyspnea.
[edit] Hemoptysis
- Hemoptysis is the coughing up of blood.
- Mitral stenosis is an important cuase of hemoptysis.
- More in chapter 13.
[edit] Cyanosis
- Differential cyanosis is when cyanosis is seen only in the lower extrimities.
- Differential cyanosis is related to a right-to-left shunt (usually through a patent ductus arteriosus).
- Right-to-left shunt at the ductus arteriosus usually results from pulmonary hypertension.
- Cyanosis occurs only in the lower extremities because blood from the pulmonary artery (deoxygenated) mixes below the carotid / subclavian (which would take the blood to the head / arm).
[edit] Interpret the symptoms of cardiac disease from a clinical scenario
[edit] Apply the components of the physical exam of the heart to a patient
[edit] Inspection
- Xanthomata are deposits of stony-hard, slightly yellowish masses found on extensor tendons of fingers.
- Pathognomonic for hypercholesterolemia.
- Think plantar and tendons of the soles of the feet.
- Primary biliary cirrhosis can lead to extremely high levels of cholesterol and therefore xanthomas.
- Antimitochondrial antibodies is found in 90% of patients with primary biliary cirrhosis.
- Eruptive xanthomata are seen in hyperlipidemia and are characterized as being on the chest, buttocks, abdomen, back, face, and arms.
- These are elevations of serum triglycerides to levels near 1500 mg / dL.
- Erythema that is disc shaped with raised edges is called erythema marginatum and can indicate acute rheumatic fever.
- Osler's nodes are painful lesions at the tufts of the finger and toes that indicate infective endocarditis.
- Splinter hemorrhages have a low specificity; they can indicate trauma, poor oxygenation, or endocarditis.
- Supravascular aortic stenosis can be characterized by wide set eyes, strabismus, low-set ears, upturned nose, and hypoplasia of the mandible.
- Pulmonic stenosis can be indicated by moon facies and widely spaced eyes.
- Hypothyroidism commonly manifests as puffy eyelids, stoic expression, and loss of the outer third of the eye brows.
- Lichtstein's sign is a lateral earlobe crease that may indicate CHD in pts over 50 yo.
- High cholesterol and / or protein levels show up in the eye as xanthelasma, though this is less specific than xanthomas.
- Arcus senilus in pts younger than 40 should raise suspicion regarding hypercholesterolemia.
- Sarcoidosis leads to opacity of the cornea.
- Marfan syndrome often produces lens dislocation.
- A high palatal arch in the mouth may indicate congenital heart disorders like mitral valve prolapse.
- Petechia on the palate may suggest infective endocarditis.
- Webbing of the neck may indicate Turner syndrome (single X, girls) which has increased risk for coarctation of the aorta.
- Webbing may also be associated with Noonan's syndrome which is associated with pulmonic stenosis.
- External chest deformations like pectus excavatum or pectus carnatum may indicate underlying cardiac development issues.
- As in Marfan's syndrome.
- An extra finger, toe, or phalanx is sometimes seen with atrial septal defects.
- Long, slender fingers are associated with Marfan's syndrome which is associated with cardiac issues.
[edit] Blood Pressure Assessment
- When using a sphygmomanometer, one is measuring the appearance and disappearance of the Korotkoff sounds.
- The point of hearing the first sounds indicates the systolic pressure.
- The point of hearing only muffled sounds indicates the top pressure range of the diastolic pressure.
- When the point of muffled and the point of not-even-muffled is more than 10mgHg apart, the point of only muffled sounds is more accurate.
- The point of hearing not even muffled sounds indicates the lower pressure range of the diastolic pressure.
- Blood pressure should be recorded at the nearest 5mmHg because all sphygmomanometers have a +/- 3mmHg accuracy.
- Ausculatatory gap occurs in hypertension; it is the disappearance of the Korotkoff sounds and then reappearance before finally disappearing at the diastolic pressure interval.
- Retake the blood pressure at the end of the examination when the pt may be more relaxed.
- Orthostatic hypotension is a drop of blood pressure by more than 20mmHg upon standing (and is associated with dizziness or syncope).
- Supravalvular aortic stenosis is indicated by hypertension in the right arm and hypotension in the left arm.
- Coarctation of the aorta is indicated by leg blood pressures that are lower than those of the arms.
- Recall that a blood pressure can be taken at the thigh / knee (with auscultation at the popliteal artery in the popliteal fossa) or at the leg / ankle (with auscultation at the dorsalis pedis or posterior tibial arteries).
- Check for infant femoral pulse to screen for coarctation of the aorta.
- Cardiac tamponade is indicated by paradoxical pulse: a difference in systolic pressure greater than 10mmHg when heard only at rest and when heard only upon inspiration.
- To test: while taking decreasing the pressure of the sphygmomanometer with the pt breathing normally, note the pressure at which Korotkoff sounds are heard only upon expiration and then the pressure at which sounds are heard only upon inspiration.
- Paradoxical pulse can also be heard in pericardial effusions, constrictive pericarditis, and increased ventilatory effort (asthma, emphysema).
| Observation | Example | Associated disease state |
|---|---|---|
[edit] Arteriole Pulse
[edit] Jugular Venous Pulse
[edit] Percussion
[edit] Palpation
[edit] Ausculation
[edit] Clinically correlate the symptoms and physical exam findings pertaining to the heart
[edit] Give a diagnosis and/or differential diagnosis based on symptoms and/or physical exam findings of the heart
[edit] Describe findings from the history and physical exam in the written history and oral case presentation
[edit] Chapter 20
[edit] Shoulder
- Describe the joint motions
- Describe the physical examination
- Differentiate diseases based on clinical features
[edit] Knee
- Describe the joint motions
- Extension 15, flexion 135, medal / lateral rotation 10
- Patellar glide 1/4 of its width.
- Describe the physical examination
- Differentiate diseases based on clinical features
[edit] Wrist
- Describe the joint motions
- Describe the physical examination
- Differentiate diseases based on clinical features
[edit] Hand
- Describe the joint motions
- Describe the physical examination
- Differentiate diseases based on clinical features




