Dermatology - Blistering Dermatoses
From Iusmicm
Contents |
[edit] Blistering Dermatoses
- Blistering diseases include:
- Contact dermatitis
- Herpesvirus infections
- Herpes simplex
- Varicella-zoster
- Major autoimmune bullous diseases
- Bullous pemphigoid
- Pemphigus vulgaris
- Dermatitis herpetiformis
- Note that these autoimmune diseases are far less common than herpes / zoster and contact dermatitis
- One should consider at what level of the integument a blister is formed: intraepidermal or subepidermal
[edit] Contact Dermatitis
- Contact dermatitis can be initiated by irritants or allergens
- Irritant dermatitis:
- Toxic injury to skin by a chemical
- In irritant dermatitis there are direct but nonspecific effects
- Less common, but often exuberant in response
- No immune response
- Allergic dermatitis:
- Allergic dermatitis is an immunological reaction to an antigen
- T-cell mediated
- A type-4 sensitivity
- Once exposed, can become sensitized; further exposures will always lead to a reaction (even when small or short in amount or duration, respectively)
[edit] Irritant Contact Dermatitis
- Strong and weak irritants generate different skin lesions
- Strong irritants: generate vesicles (small) or bullae (large) within 24 hours
- Examples are battery acids, bases
- Weak irritants: generate dry, scaly eruptions
- May be more severe at intertriginous areas
- Require repetitive exposures to cause eruptions
- Examples are detergents, personal care products
- Strong irritants: generate vesicles (small) or bullae (large) within 24 hours
- Pathogenesis of irritant dermatitis: a direct toxic effect is observed on the skin
- Examples of irritants: acids, alkalis (bases), solvents, detergents
[edit] Allergic Contact Dermatitis
- Allergic contact dermatitis (unlike irritant dermatitis) requires an initial sensitization to the antigen, called the primary sensitization.
- A rash occurs 7-21 days after the primary exposure (sensitization).
- Secondary exposures result in rashes within 24-48 hours.
- Examples include: poison ivy (urushiol), nickel, rubber compounds, paraphenylenediamine, ethylenediamine
- Paraphenylenediamine: used as a hair dye, used in production of rubber materials, used in camera film development
- Ethylenediamine: used in production of many industrial chemicals, a preservative, found in some personal care products
- The "itch" complaint over pain or burning should lead you to consider contact dermatitis.
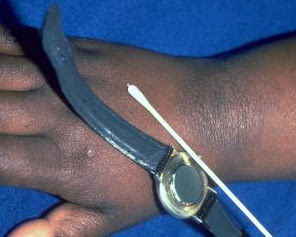
- Often we test for allergy to stuff with a patch dusting: applying antigens to the skin of the back and watching for a urushiol-like reaction.
- The "true" test is a panel of 27 antigens that are common agents of allergy.
[edit] Pathogenesis of allergic contact dermatitis
- A delayed hypersensitivity reaction (by the immune system)
- Primary exposure: antigen binds with a skin protein, langerhans cells are sensitized, T cells develop against the hapten product
- Recall that langerhans cells reside in the dermis, especially in the papilla of the DEJ (dermal-epidermal junction).
- Note that many allergic contact dermatitis agents require an endogenous protein product to act as an hapten (a protein that binds the antigen, making it detectable as foreign by langerhans cells and thus antigenic).
- Recall that langerhans cells with an antigen bound will travel down the afferent lymph to a lymph node to interact with and activate CD4+ T cells (in the paracortex of the node).
- Secondary exposure: T cells react quickly to the antigen
- Upon second exposure, langerhans cells are able to activate some CD4+ T cells residing at the site of exposure via IFN-gamma before every migrating to the lymph node.
- Upon activation by langerhans cells at the lymph nodes, CD4+ T cells will migrate to the site of the antigen exposure via arteries.
- It is the edema effect that generates blisters!



[edit] Histology of allergic contact dermatitis
- Intercellular edema (also called spongiosis)
- Intraepidermal vesicles
- Lymphocytic and eosinophilic dermal infiltrate





[edit] Common causes of allergic contact dermatitis
- Poison ivy, poison oak, poison sumac
- Nickel
- Perfumes
- Rubber compounds

[edit] Herpesvirus Infection Blistering Dermatitis
- Herpesvirus can cause blistering dermatitis as the herpes simplex virus or as the latent varicella-zoster virus
- Primary herpes infections:
- The primary infection is much more severe with vesiculations, more edema, eruption of the lesions, etc.
- With primary there can be fever, malaise, etc.
- Herpes can be life-threatening for infants / children, especially if they get herpes encephalitis.
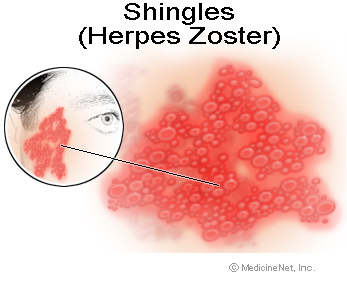
- Varicella zoster
- Must have been exposed earlier in life to primary herpes simplex infection
- Could also arise after vaccination
- Recall that zoster resides in the DRG
- Varicella zoster produces monomorphic vesicles: that is, all the vesicles are in the same phase.
- Recall that chickenpox (the primary infection) is marked by vesicles at different stages.
- Recall that zoster can arise in one dermatome or one side or many dermatomes bilaterally.
- Examples of herpes simplex:
- Examples of varicella zoster:
- Histology of herpesvirus infections causing dermatitis:
- Infected cells manifest as large "ballooned" cells
- Multinucleated giant cells are found as macrophages eat up host cells
- Intraepidermal vesicles are present (as with other bullous dermatitis states like allergic contact dermatitis and irritant contact dermatitis)


- The Tzanck preparation (test) can be used to test for herpes infection
- The procedure involves: unroofing a blister / vesicle, scraping the base of the blister / vesicle, smear scraped material on a slide, stain with zinc or copper stain, examine via microscope.
- Tzanck cells (multinucleated giant cells) are the key finding generating a positive test and a diagnosis of herpes.
- Note that the Tzanck test will not tell you if this is a herpes infection or a zoster infection.
[edit] Auto-immune Blistering Dermatoses
- Autoimmune blistering dermatoses are classified by the location of the bullae.
- This is a useful distinction because intraepidermal blisters are observed as being flaccid and subepidermal blisters are observed as being tense.
- Flaccid blisters are more readily broken open than tense blisters.
- Intraepidermal blistering autoimmune diseases include pemphigus vulgaris
- Subepidermal blistering autoimmune diseases include bullous pemphigoid and dermatitis herpetiformis
- Recall that bullae are a curcumscribed collection of free fluid > 0.5 cm.
- Vesicle is < 0.5 cm.
[edit] Pemphigus vulgaris
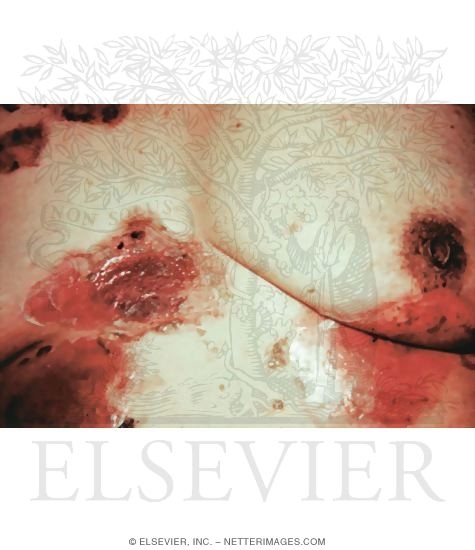
- Pemphigus vulgaris is an intraepidermal autoimmune reaction that generates flaccid bullae.
- Vulgaris tends to show up on the oral mucosa, the scalp, and the intertriginous areas
- Vulgaris was a fatal disease before we had corticosteroids as a treatment option
- PV generates flaccid bullae that are often pulled down by gravity; there is often a brown crusting (soggy cornflakes).
- Pathogenesis of pemphigus vulgaris:
- Self antibodies bind to the membrane of skin cells, inducing release of inflammation mediators
- Inflammation mediators lead to inflammation and acantholysis
- Acantholysis: a breakdown of the skin cell layers
- As the skin breaks down and fluid accumulates (secondary to inflammation mediators) a blister forms
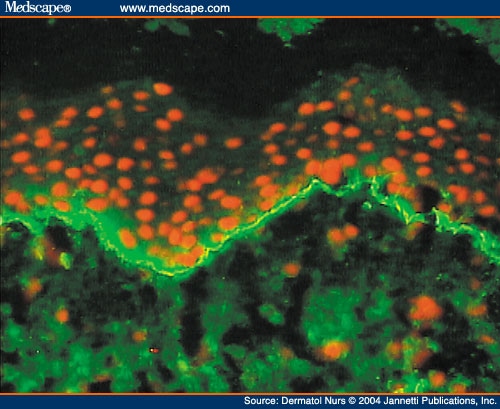
- Immunofluorescence of pemphigus vulgaris:
- Direct versus indirect:
- Direct: take tissue, incubate with mouse antibodies against human antibodies; localizes autoimmune activity of host antibodies on host tissue
- Indirect: take serum, incubate with animal skin, identify where antibodies localize on foreign tissue; localizes autoimmune activity of host serum antibodies in a foreign tissue
- Endogenous, circulating IgG immunoglobulin are directed against the cell membrane of keratinocytes
- Thus self-Ig is deposited between the keratinocytes
- Immunofluorescence demonstrates a characteristic staining pattern (see below)
- Direct versus indirect:
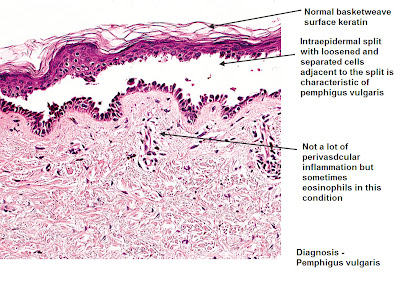
- Histology of pemphigus vulgaris:
- Pemphigus vulgaris is marked by basal keratinocytes clinging to the basement membrane (b/c autoimmune rxn is between keratinocytes not at the bm) and circulating immune cells in the dermis just deep to the basement membrane (making the antibodies)



[edit] Bullous Pemphigoid
- Bullous pemphigoid is a subepidermal autoimmune reaction that generates tense bullae.
- Note that pemphigus vulgaris is intraepidermal and generates flaccid bullae.
- Bullous pemphigoid can be found anywhere on the body but is unlikely to occur on mucosal surfaces.
- Note that pemphigus vulgaris is primarily found on the scalp, in the mucosal membrane, and in the intertriginous areas.
- Bullous pemphigoid can be characterized by a pruritis (itching).
- Bullous pemphigoid is associated with the elderly.
- Pathogenesis of bullous pemphigoid:
- Self antibodies bind to the basement membrane of the epidermis, inducing release of inflammatory mediators
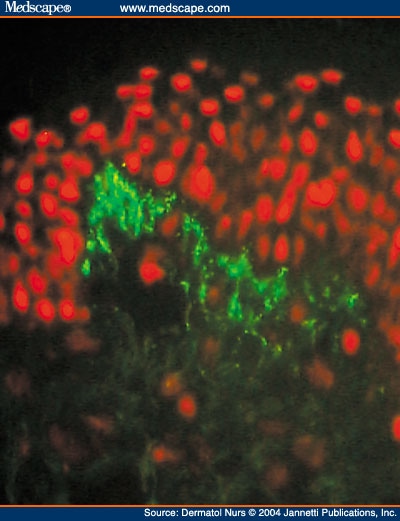
- Immunofluorescence of bullous pemphigoid:
- Endogenous, circulating IgG immunoglobulins are directed against the basement membrane of the epidermis
- Thus self-Ig is deposited along the basement membrane
- Immunofluorescence demonstrates a characteristic staining pattern
- There is an urticative phase in BP: it will be an itchy plaque
- Histology of Bullous pemphigoid
- Note that there will be no keratinocytes at the bm because that's where the autoimmune rxn is occurring.
[edit] Dermatitis Herpetiformis
- Dermatitis herpetiformis is a subepidermal autoimmune reaction that generates tense bullae.
- Dermatitis herpetiformis is associated with young adults (3rd and 4th decade).
- Recall that bullous pemphigoid is associated with the elderly.
- Dermatitis herpetiformis generally shows up on the elbows, knees, buttocks, and upper back.
- Recall that pemphigus vulgaris is usually on the oral mucosa, the scalp, and the intertriginous areas.
- Recall that bullous pemphigoid can be found anywhere on the body.
- Dermatitis, just like bullous pemphigoid, can produce pruritis.
- Dermatitis usually presents as a cluster of vesicles.
- That is, there are usually many smaller blisters as opposed to bullous pemphigoids fewer, larger blisters (bullae).
- Often the vesicles are scratch off so they are not observed
- Dermatitis herpetiformis is an hypersensitivy reaction to dietary gluten
- However, dermatitis herpetiformis does not necessarily co-manifest with gluten-sensitive enteropathy (Celiac disease).
- Pathogenesis:
- Antigen-antibody complexes are deposited at the EDJ (epidermal-dermal junction), induce inflammatory response
- Inflammation results in a subepidermal vesicle and pruritis
- Immunofluorescence:
- Endogenous, circulating IgA immunoglobulins bind with antigen and form complexes at the EDJ.
- These complexes are in granules and thus form a characteristic pattern distinct from bullous pemphigoid or pemphigus vulgaris.
- Note that the small granules of immunofluorescence are often at the tip of epidermal-dermal papilla


- Histology of dermatitis herpetiformis
- Neutrophils in little vesicles
- IgA is deposited at the BM (in the papilla tips)