Dermatology - Benign Tumors and Premalignant Changes
From Iusmicm
Contents |
[edit] Benign tumors
[edit] Seborrheic keratoses (SK)
- Epidemiology of seborrheic keratosis:
- the most common cutaneous neoplasm
- unusual in children
- increases in incidence with age (not-rare in children, very common in elderly)
- no diff in gender
- Etiology of seborrheic keratosis: unknown
- Distribution:
- any cutaneous surface but not the mucous membrane
- primarily on the trunk (may have Christmas tree pattern)
- The long axis of a seborrheic lesion is oriented along skin lines
- Appearance of seborrheic keratosis:
- 1-2mm to 1-2cm in diameter
- Yellow to dark brown
- Macular or papular
- Velvety or verrucous (thickened and scaly; wart-like) in texture
- Stuck-on appearance
- May appear greasy



- Symptoms of seborrheic keratosis:
- Usually asymptomatic
- Occasionally pruritic
- May become irritated if rubbed by a shirt, bra, collar, etc.
- Variants of sebhorreic keratosis:
- Stucco keratoses: elderly; acral areas; 3-4 mm seborrheic keratoses; appear gray-white in color; asymptomatic
- Dermatosis papulosa nigra: in people with darker skin tones, on the face, multiple tiny seborrheic keratosis
- Note that stucco keratoses has large seborrheic keratoses while papulosa nigra has smaller seborrheic keratoses.
- Stucco keratoses: elderly; acral areas; 3-4 mm seborrheic keratoses; appear gray-white in color; asymptomatic
- Treatment
- No treatment is generally needed; tx is initiated if irritated or for cosmetic reasons
- Cryotherapy: freeze with liquid nitrogen
- Electrosurgery: electrodesiccation for small lesions
- Chemical peels: flattens and lightens the lesions
- Laser: CO2 or Erbium:Yag vaporizes the lesions
[edit] Nevi
- Nevi are benign proliferations nof melanocytes in the skin.
- Epidemiology of nevi:
- Prevalence varies with age
- Prevalence increases with lighter skin
- Very common: 20x20: 20 nevi by 20yo in Caucasians
- Etiology of nevi:
- Unknown
- Nevi are probably related to cumulative UV light exposure
- Painful sunburns before 20yo are associated with increased nevi development
- Use sunscreen! It decreases new nevi in children
- May have a genetic component
- Risk factors
- Distribution: any cutaneous surface
- In kids, tends to be in sun-exposed areas
- Appearance:
- Nevi are usually orderly: symmetrical, regular borders (round / oval), homogenous color, homogenous surface texture
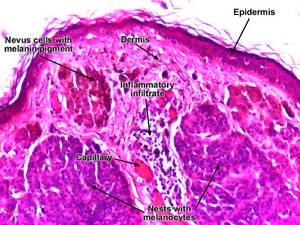
- Nevi come in several types: junctional, compound, or intradermal depending on their location in the epidermis / dermis
- These types (junctional, compound, or intradermal) are used in pathologic descriptions and correlate with clinical appearance
- Junctional nevi: nests of cells at the EDJ (epidermal-dermal junction); small (1mm - 1cm), round, flat (or slightly raised), light / dark brown / black
- Compound nevi: nests of cells at the junction AND in the dermis; raised, papillomatous, skin-colored / light tan / brown / black
- Dermal nevi: nests of cells are only in the dermis; raised (papules, may even be pedunculated or dome shaped), smooth or papillary surface, rubbery texture, flesh to brown
- Type can change with normal life-cycle.
- Note that compound nevi have the widest range of color.
- Note that the deeper the nevus cells, the more raised the lesion: junctional nevi are flat or very slightly raised (at EDJ), compound nevi is (slightly) raised (at EDJ and dermis), dermal nevi are domed / pedunculated (at the dermis).



- Pathogenesis (life cycle):
- Nevi have a life cycle of appearance and regression
- Nevi appear in months 6-12 of life
- Nevi then increase in number and size in early childhood, puberty, and 2nd / 3rd decades
- Recall that sun exposure increases risk
- Nevi then regress later in life (eventually disappearing)
- Nevi can have eruptive growth during adolescence, pregnancy, or with steroid / hGH use
- Diagnosis of nevi:
- Family history of melanoma should be queried
- Check the ABCDEs: asymmetry, (irregular) border, (jet-black or variegated) color, (increasing) diameter (or over 6mm; pencil eraser), (increasing) elevation
- Also ask about itchiness, pain, or irritation
- When in doubt, biopsy!: use a punch or excisional biopsy to get the best measurement of height from the granular cells.

- Treatment of nevi:
- Most require no treatment at all
- Might excise for cosmetic reasons or if they become irritated
[edit] Cysts
- A cyst is any round to dome-shaped, mobile lesion that contains expressible material
What does "expressible mean"?
- Epidemiology of cysts:
- Extremely common
- Male:Female::2:1
- Etiology of cysts:
- Usually idiopathic
- May come from an occluded follicular infundibulum (section of hair follicle above the sebaceous gland)
- May come from traumatically implanted epidermis as in surgical scars
- May be a growth of skin-within-the-skin.
- Distribution of cysts: mainly the face (especially the preauricular area), neck, and chest
- Appearance of cysts:
- Usually flesh-colored papules or nodules (commonly dome-shaped)
- 1-2mm to 1-2cm
- Often has small central punctum connectin gthe cyst to the epidermis



- Symptoms of cysts:
- May become infected or inflammed
- Treatment:
- Excision: surgery can be used to remove the cyst wall; recurrence if entirety of wall isn't removed
- Manage complications (infected cysts): warm compresses (increases blood flow and immune access), incise and drain, antibiotics against skin flora (cloxacillin, erythromycin, cephalexin)
- Be careful if the pt has heart valve infections because treatment of cysts may release pathogens into the blood and cause endocarditis.
[edit] Premalignant changes
[edit] Actinic keratoses
- Actinic keratosis is a pre-malignant lesion of keratinocytes
- Epidemiology of AK:
- Usually occurs in fair-skinned individuals
- Usually begins in 30s-40s
- Elderly: 50%
- Hot / sunny areas: 50%, younger onset (teens and 20s)
- Develop over time
- Risk factors of actinic keratosis:
- Fair skin
- Older age
- Blue eyes
- Red or blond hair
- Outdoor occupation or recreation
- Childhood freckling
- Distribution: sun exposed areas
- When on the mucosa (lips), called actinic cheilitis
- Appearance of actinic keratosis:
- Color: flesh to erythematous
- Ill-defined macule to papule: sometimes better felt than seen
- Dry, adherent scaling
- Sometimes better felt than seen
- Size: pinhead diameter to several cm
- Usually multiple lesions





- Symptoms: usually asymptomatic
- Variants
- Actinic cheilitis (lips)
- Usually on the lower lips
- Lesions have: scaling (diffuse and slight); commissures (sometimes over the entire lower lip); may show up as leukoplakia
- Background skin has: blotchy, atrophic appearance; an indistinct and irregular vermillion with perpendicular wrinkles,
- Actinic cheilitis (lips)
- Treatment of actinic keratosis:
- AK can be treated with direct destruction or chemotherapy
- Destructive modalities: liquid nitrogen, curettage, chemical peels, laser ablation
- Curettage: physical scraping removal via curette
- Chemical peel: chemical treatment that causes superficial layers to slough off
- Chemotherapy: Topical 1-5% 5-fluorouracil; lights up subclinical lesions
- PDT: photodynamic therapy
- Paint on a photosensitizer (chemical)
- Pre-malignant cells uptake the chemical (more than other cells; takes several hours)
- Hit with UV light to turn photosensitizer chemical into superoxide radicals
- Death of pre-malignant cells