Exam 1 PD Objectives
From Iusmicm
Revision as of 21:59, 26 January 2012 by 134.68.138.157 (Talk)
Lange: Chapter 1: I Have a Patient with a Problem: How do I figure out the possible causes?
- Pages 1-9
- Define the steps in the diagnostic process.
- Define sensitivity, specificity and likelihood ratio.
- Understand how true negatives, false negatives, false positives and true positives are determined.
Chapter 8: Chest Pain
- Pages 130-148
- Know the differential diagnosis of chest pain by anatomical organization.
- Know the key factors in the history and on physical examination and initial diagnostic evaluation that accompany each of the following diagnoses:
- Stable Angina
- GERD
- Myocardial Infarction
- Unstable Angina
- Aortic Dissection
- Pleural Effusion
- Acute Pericarditis
Chapters 13 & 14: The Chest and the Cardiac Examinations
- Pages 362-390, Pages 391-437
Chapter 15: Peripheral Vascular System
- Pages 438-454
- Define and describe the components for the physical examination of the peripheral vascular system.
- Unlikely to be a test question; just watch the video.
- Differentiate ulcers caused by arterial insufficiency and venous insufficiency.
- Arterial insufficiency ulcers: cool / pale limb with painful, rapid onset, punched out, crusted lesions on the heels and toes.
- Venous insufficiency ulcer: warm / erythematous limb with painless (early at least), insidious, diffuse, reddened, thickened lesions superior to the medial maleolus.
- Define and differentiate intermittent claudication and pseudoclaudication.
- Intermittent claudication is unilateral (usually) pain in the lower limb upon exertion and worsened by cold temperatures or elevation.
- Claudication pain is usually in the calf, arch of the foot, thighs, hips, or buttocks.
- Pseudocladucation is bilateral numbness or pain in the legs that results from musculoskeletal pathology in the lumbar area.
- Intermittent claudication is unilateral (usually) pain in the lower limb upon exertion and worsened by cold temperatures or elevation.
- Differentiate skin changes caused by arterial insufficiency and venous insufficiency.
- Arterial insufficiency is marked by paleness and coolness (no blood / warmth gets there).
- Venous insufficiency is marked by warmth, erythema, and excoriations (from scratching at pruritis).
- Identify important risk factors for the development of thrombus formation.
- Anything that causes or increases blood stasis increase the risk of thrombus formation.
- Risk factors for thrombus formation include: bed rest, congestive heart failure, obesity, pregnancy, extended airplane travel, and oral contraceptives.
- Recognize the symptoms of emboli affecting various organ systems.
- Pulmonary embolic symptoms: shortness of breath (think pulmonic arteries)
- Abdominal embolic symptoms: pain (think splenic, intestinal, and renal arteries)
- Neuro embolic symptoms: syncope, confusion, coma etc. (think carotid and vertebrobasilar arteries)
- Peripheral embolic symptoms: pain and paresthesias (think brachial artery, etc.)
- Clinically correlate abnormal findings when found on the examination of the arterial system. The student should be able to correlate and interpret the physical finding with the following disease processes:
- S&S of abdominal aortic aneurysm: a laterally expansive pulsatile mass may be palpated, abdominal bruit, femoral bruit, femoral pulse deficit, pain (in the back and abdomen, upon rupture).
- Be careful not to interpret a normal aorta in the thin pt as an aneurysm.
- Auscultate for AAA 2 inches above umbilicus, at midline.
- Abdominal bruits heard only during systole are usually not pathologic.
- S&S of renal artery stenosis: auscultated bruit (99% specificity, 39% sensitivity)
- A renal bruit is considered combined systolic-diastolic and is found 2 inches above and 2 inches lateral to the umbilicus.
- S&S of coarctation of the aorta: delayed femoral pulse as compared to radial pulse.
- Recall that the femoral pulse should arrive just before or at the same time as the radial pulse in normal physiology and anatomy.
- Be especially suspicious of coarctation of the aorta in hypertensive individuals.
- S&S of obstructive aortoiliofemoral disease: delayed / diminished comparison of femoral pulses, femoral bruit.
- S&S of atherosclerosis of the carotid artery: carotid bruit may be auscultated (with pt in supine position with head on pillow), carotid murmur may be auscultated (can also be a loud murmur from the heart)
- S&S of peripheral vascular disease: decreased pulses, excessive / prolonged pallor, poor reperfusion, incompetent saphenous vein.
- Recall, also, the five p's: pain, pallor, paresthesia, paralysis, and pulselessness.
- S&S of abdominal aortic aneurysm: a laterally expansive pulsatile mass may be palpated, abdominal bruit, femoral bruit, femoral pulse deficit, pain (in the back and abdomen, upon rupture).
- Define and differentiate generalized lymphadenopathy, localized lymphadenopathy, lymphangitis, and lymphedema.
- Generalized lymphadenopathy: the presence of palpable lymph nodes in three or more lymph node chains.
- Generalized lymphadenopathy suggests a systemic diagnosis like lymphoma, leukemia, collagen vascular disorders, and systemic bacterial / viral / protozoal infections.
- Localized lymphadenopathy: the presence of palpable lymph nodes in less than three lymph node chains.
- Localized lymphadenopathy suggests a localized infection or neoplasm.
- Lymphangitis: lymphatic spread of infection or neoplasm manifesting thin, red streaks on the skin.
- Recall the fungus Sporothrix schenckii which is common is gardners and florists that get pricked by rose thorns. It works its way up the lymphatics of the arm, leaving a string of ulcers or nodules.
- Lymphedema: resulting from obstruction of lymphatic drainage, this type of edema is usually firm and non-pitting as compared to vascular edema which is usually pitting.
- Generalized lymphadenopathy: the presence of palpable lymph nodes in three or more lymph node chains.
- Define and appropriately apply the Allen test on a patient. The student should be able to interpret the findings of this test.
- The Allen test detects arterial insufficiency in the upper extremities, specifically the ulnar and radial arteries.
- The test is based on expected, normal refill when either the ulnar or radial artery are compressed and the hand is emptied of blood (pt makes a fist).
- If, upon opening the fisted hand, there is delay of refilling, the opposing artery may be insufficiency. (That is, if you compress the radial artery, have the pt make a fist, have them open it, and observe poor refilling, then the ulnar artery may be insufficient).
- The Allen test!
Chapter 16: Breast
- Pages 455-476
- Differentiate the clinical significance of a lump that enlarges during the premenstrual and menstrual stages of the cycle and the breast lump which does not change during the menstrual cycle.
- A breast lump that enlarges during premenstrual / menstrual stages is likely physiological nodularity
- Describe and identify the changes of the skin and nipple which are strongly suggestive of neoplasm.
- Characteristics associated with neoplastics changes of the breast include nipple discharge, nipple inversion, skin changes overlying a mass.
- Describe the different types of nipple discharge. Differentiate and identify the different types of nipple discharge and their clinical significance.
- Types of nipple discharge include: serous (thin, watery, yellowish), bloody, and milky.
- NB: both serous and bloody types of discharge can be associated with malignancy so the the presence of discharge is more important than the type of discharge.
- Serous discharge commonly results from intraductal papilloma in one of the large subareolar ducts, with oral contraceptive use, or with carcinomas.
- Bloody discharge commonly results from intraductal papilloma (as with serous discharge), too.
- Describe the components of the physical examination of the breast and the proper positioning of the patient for each component.
- The components of the breast PE include inspection (seated; hands on hips; hands pulling apart a shoulder level; hands above head; leaninig forward), axillary examination (pt seated; arm held up away from axilla), and paplation (pt lying; hand above head; shoulder on table; potentially leaned toward opposite side to distribute breast over chest wall).
- Describe the following changes of the breast: erythema, edema, and dimpling. Identify and describe the differential diagnosis for each of the above physical findings.
- Erythema: Erythema is an important symptom of breast carcinoma.
- Edema: Edema is characterized by the prominent pores and is an important sign of malignancy called peau d'orange. (Lymphatics are clogged by emboli of tumor tissue.)
- Dimpling: The presence of dimpling warrants further investigation.
- Describe the proper physical exam technique for axillary examination. Describe and name which lymph node regions that should be palpated on physical examination.
- With the pt seated and arm abducted away from the body (lay arm over examiner's shoulder), pectoral muscle relaxed, make dime-size circles with the pads of the fingers (without losing contact with the skin), working superiorly. Palpate the anterior and posterior aspects of the axilla. Adduct the arm as one moves superiorly to allow for deep, superior palpation.
- Palpate the supraclavicular nodes and infraclavicular nodes.
- Freely moving nodes (3-5 mm) are common and usually due only to lymphadenopathy.
- Describe the characteristics which should be used to describe a breast mass which is found on physical examination.
- Skin condition, symmetry, dimpling, masses, discharge, and lymphadenopathy should all be addressed.
- Skin should be described in color and texture.
- Discharge should be characterized by consistency and color.
- Dimpling should be described as location on the clock and from the nipple.
- Masses should be described in size and texture.
- Nodes should be described in motility and texture.
- Based on a clinical description, differentiate between cystic disease, a benign adenoma, and a malignant tumor.
| Trait | Cystic Disease | Benign Adenoma | Malignant Tumor |
|---|---|---|---|
| Pt Age | 25-60 | 10-55 | 25-85 |
| # of masses | 1+ | 1 | 1 |
| Shape | Round | Round | Irregular |
| Consistency | Elastic, soft, hard | Firm | Stony hard |
| Delimitation | Well delimited | Well delimited | Poorly delimited |
| Mobility | Mobile | Mobile | Fixed |
| Tenderness | Tender | None | None |
| Dimpling | None | None | Dimpled |
- Note that malignant tumor traits have low sensitivity:
- Mobility fixed: 90% spec, 40% sens
- Poorly delimited: 90% spec, 60% sens
- Consistency hard: 90% spec, 62% sens
- 50% of fixed masses are cancerous; 60% of fixed, irregular masses are cancerous;
- Classic description of a benign mass is mobile, well circumscribed, soft or cystic.
- Classic description of a cystic mass is multiple, tender, mobile, elastic (soft or firm), well circumscribed.
Chapter 19: Female Genitalia
- Pages 549-583.
- Identify and describe the components of the physical examination of the female genitalia.
- Too long. See outline given at SPD.
- Recognize abnormalities that can be found on each component of the exam.
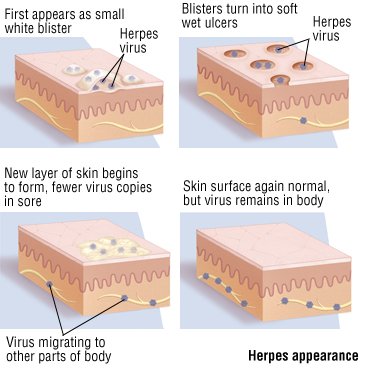
- Recognize and differentiate the clinical features of genital ulcerations.
- The three primary genital ulcerations are: herpes (HHV), syphilis (T. pallidum), and chancroid (Haemophilus ducreyi).
- Distict features of sphyilis: long incubation time (9-90 days), a single ulcer, painless, rarely recurrent.
- Distict features of herpes: vesicular, heals within 2 weeks
- Distict features of chancroids: multiple papules / pustules.

- Painful (herpes, chancroid) -> vesicle (herpes), papule / pustule (chancroid)
- Painless (syphilis)
- Multiple ulcers (herpes, chancroid) -> (
- Describe and give recommendations for screening for cervical cancer for a patient based on the American cancer Society recommendations.
- Beginning at 21yo, screen with Pap smear (or every 2 years with liquid-based prep).
- Beginning at 30yo (with three normal, consecutive paps and no complicating factors like hx of STIs), screen with Pap smear every 2 or 3 years. One can also screen in these conditions every 3 years (but not more frequently) with the HPV DNA probe.
- Beginning at 70yo (with no abnormal paps in the last 10 years and no complicating factors like recent hx of STI), one can discontinue screening.
- Define and recognize the following sequelae of pelvic floor relaxation: cystocele, rectocele, and uterine descent.
- Define and differentiate the following: amenorrhea, menorrhagia, metorrhagia, menometrorrhagia, and postmenopausal bleeding.

- Post-menopausal bleeding occurs...after menopause.
Chapter 22: Integrating the exam
- 696-706


