Cardiology - Aortic Valve Disease
From Iusmicm
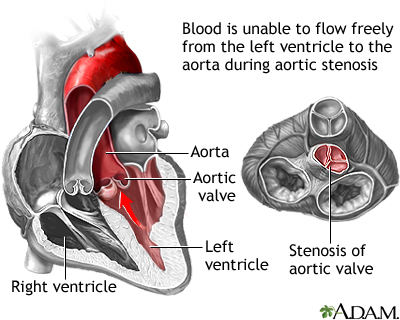
Aortic Stenosis
- Recall that "stenosis" is a narrowing.
- Sclerosis is a hardening (decrease in compliance).

A Case
- 67 yo woman referred for murmur which she has known about for a ‘few years.’
- Over recent months she has noticed dyspnea climbing stairs– before she was completely asymptomatic.
- On exam, BP 140/86. JVP appears normal. Carotid upstroke is mildly diminished and delayed. Chest clear to auscultation. Cardiac exam with III/VI systolic ejection murmur at RUSB radiating to carotids and apex
which is late peaking. No diastolic murmur is heard. The PMI is sustained and a soft S4 is heard at the apex.
- Why is the carotid upstroke delayed and diminished?
- What is the underlying valvular pathology and how severe is it?
- What should be done about it?
Aortic Stenosis: Underlying Causes
- Aortic stenosis can result from four underlying causes: calcification, rheumatic disease, congenital malformations (bicuspid, unicuspid), and radiation treatment.
- For pts < 70 yo, the major causes of aortic stenosis are bicuspid, rheumatic, and calcification.
- For pts > 70 yo, the major causes of aortic stenosis are calcification, bicuspid, and rheumatic.

Aortic Valve Sclerosis
- Recall that in general, sclerosis is a decrease in compliance due to thickening or scarring.
- Specifically we say "sclerosis is a focal thickening of valve cusps with normal excursion and no obstruction to flow".
- The pathophysiology of a sclerotic valve is similar to atherosclerosis (think plaques, ulcerations, clotting, etc.)
- Aortic valve sclerosis is a normal development with age as 25% of pts over 65 yo have a sclerotic aortic valve.
- NB: aortic valve sclerosis may progress to aortic stenosis.
- In addition, sclerotic aortic valves double the risk of coronary events.
- Sclerotic aortic valves generate an early peaking systolic ejection murmur (SEM) at the right upper sternal border (RUSB).
- This murmur is a function of normal flow over abnormal anatomy.
- The longer the systolic murmer (decrescendoing), the worse the stenosis





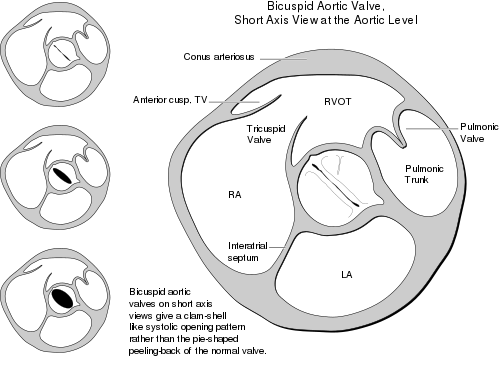
The Bicuspid Aortic Valve
- Bicuspid aortic valves are found in 1-2% of the population.
- Bicuspid aortic valves are 4 times more common in males.
- Like aortic valve sclerosis, a bicuspid valve can lead to stenosis.
- In addition, an aortic bicuspid valve can produce regurgitation.
- Indeed, many pts with aortic bicuspid valve will require surgery.
- Aortic bicuspid valves moderately increase the risk of endocarditis.
- The bicuspid aortic valve will produce a systolic ejection click as the two leaflets catch on each other upon opening.
- Bicuspid aortic valve (an therefore a systolic ejection click) should be a hint to check for aortic disorders:
- Ascending aortic aneurysm in 50% of pts with a bicuspid aortic valve
- Coarctation in 10% of pts with a bicuspid valve
- 30-50% with coarctation have a bicuspid aortic valve
- Aortic dissection in pts with a bicuspid aortic valve


�===Aortic Stenosis: Pathophysiology===
- The primary pathophysiology behind aortic stenosis is an elevated pressure in the left ventricle as it tries to force the same amount of blood through a smaller (stenotic) hole (aortic valve).
- An elevated pressure in the left ventricle is compensated by left ventricular hypertrophy which makes the left ventricle stronger so it can push the same volume of blood through a stenotic aortic valve.
- This type of compensation is concentric compensation because the left ventricle hypertrophies concentrically by laying down more contracile units concentrically (that is, parallel to) the exisiting units.
- Concentric hypertrophy works initially but with increasing stenosis (and therefore increasing hypertrophy) the cardiac output becomes fixed meaning the pt can no longer respond to increased effort or increased venous return by expanding the ventricle (and therefore increasing output by Starling's principle).
- Concentric hypertrophy fails as stenosis keeps rising but cardiac output declines passed an ability to sustain the pt.
The Law of LaPlace
- The law of LaPlace is about wall stress because the heart wants to keep wall stress low.
- LaPlace determined that wall stress is a function of pressure, radius, and thickness.
- More pressure, more stress.
- Larger radius, larger stress.
- More thicknes, less stress.
- Wall stress = (Pressure * Radius) / (2 * Thickness)
- Note that the Law of LaPlace applies to alveoli and vasculature, too.


Aortic Stenosis: Presenting Symptoms
- The signs and symptoms of aortic stenosis are angina, syncope, and heart failure.
- Angina makes sense in the setting of aortic valve stenosis because:
- Muscle mass is increasing (LV hypertrophy b/c must get same volume through stenotic aortic valve) and the heart muscle tissue elicits pain (angina) upon lack of oxygen.
- Coronary flow is reduced (because LV is having a hard time getting blood through aortic valve and also because there is increased resistance in vessels of LV as the muscle has hypertrophied) and the heart muscle tissue elicits pain (angina) upon lack of oxygen.
- There is usually (50% of the time) concurrent coronary artery disease (blockages in the coronary arteries) and the heart muscle tissue elicits pain (angina) upon lack of oxygen.
- Syncope makes sense in the setting of aortic valve stenosis because:
- The heart (left ventricle) can no longer increase output (because of it's concentric hypertrophy and therefore fixed output) to meet increased physical demands so the brain says "I don't have enough oxygen to work with" and shuts down.
- The brain responds to high left ventricular pressure by inducing syncope.
why?
- Heart Failure makes sense in the setting of aortic valve stenosis because:
- The left ventricle has hypertropied (concentrically) to the point of diastolic dysfunction because it is so thick (and therefore stiff).
- The heart (left ventricle) can no longer increase it's output (because concentric hypertrophy has encroached on lumenal space) such that the cardiac tissue itself begins to function with too little oxygen.
- Cardiac tissue develops systolic dysfunction because of a decreasing cardiac output (yet increasing or stable stenosis).
Aortic Stenosis: Physical Exam
- Recall that aortic stenosis is a narrowing of the LV-aortic junction.
- Recall that aortic stenosis murmurs are due to normal flow through abnormal anatomy (in this case narrowed anatomy).
- Recall that aortic stenosis can result from aortic bicuspid valve, calcification, sclerosis, and rheumatic fever.
- The physical exam findings of aortic stenosis include:
- a systolic ejection click (if stenosis is secondary to a bicuspid valve)
- an early peaking systolic ejection murmur at the RUSB that radiates to the carotids
- This is a crescendo-decrescendo shaped murmur.
- The later in systole the peak intensity, the more severe the stenosis.
- The systolic ejection murmur of aortic stenosis will be "harsh and grade II+".
- a weak and late (parvus (little) et tardus (late)) carotid pulse
- It makes sense that the carotid pulse will be weak and late because with stenosis the blood arrives at the carotid late and with decreased pressure (imagine the small whole zapping some of the normal pressure that would produce the carotid pulse).
- a sustained left ventricle apical impulse
What is apical impulse?
- a fourth heart sound (S4, due to ventricular stiffness because of concentric hypertrophy)
- (S3 may or may not be heard late in the course of aortic stenosis)
- (A2 of S2 may be decreased in severe cases).
- A decreased A2 makes sense as the aortic valve opening becomes very small the valve doesn't have far to close so the closing sound will decrease.
�Aortic Stenosis: Diagnosis
- Diagnosis of aortic stenosis is ultimately by echocardiography.
- Remember, however, that the pt should have the typical physical exam findings: crescendo-decrescendo systolic murmur, parvus et tardus carotid pulse, sustained apical impulse, and S4 (and S3 and decreased A2 in late course).
- The pt should have classic symptoms: angina, syncope, and heart failure.
- Diagnosis may also be aided by observing changes in EKG tracings and cardiac catheterization with pressure differential measured between LV and aorta.
- Recall that the primary pathophysiology of aortic stenosis is increasing pressure in the left ventricle due to decreased output tract area (stenosis).
Aortic Stenosis: Grading Severity
- Aortic stenosis is measured by the area of the junction between the left ventricle and the aorta and the pressure gradient between the LV and the aorta.
- The smaller the area, the worse (mild -> moderate -> severe).
- The larger the pressure difference, the worse (mild -> moderate -> severe).
Aortic Stenosis: Natural History
- Recall that aortic stenosis is a narrowing of the LV output tract that causes an increase in LV pressure.
- Recall that the LV undergoes concentric hypertrophy to compensate for the need for increased pressure (to get the volume through the smaller area).
- Recall that concentric hypertrophy eventually decreases the cardiac output causing symptoms.
- Recall that symptoms of aortic stenosis include syncope, angina, and heart failure.
- This process doesn't really stop and the natural history leads to a rapid progression as cardiac output decreases to a point that damages the heart tissue (which cyclically and therefore rapidly leads to worse output and more damage).
- 27-79% of pts with (mild-moderate) aortic stenosis progress ot death or surgery within 5 years.


Aortic Stenosis: Therapy
- The definitive treatment for aortic stenosis is aortic valve replacement.
- However, percutaneous aortic valvuloplasty is of limited utility in adults
- TAVI = transcatheter aortic valve implantation.
- TAVI is the up and coming treatment.
- TAVI has been shown to be as good as but not better than percutaneous valve replacement.
Therapy: Indications for AVR (aortic valve replacement)
- Pts are recommended for valve replacement based on their symptoms, LV function, and opportunity.
- Severe symptoms justify replacement.
- LV dysfunction (as defined as ejection fraction (EF) < 50%) justifies replacement.
- Another cardiac surgery provides an opportunity and justification to replace the valve.
- Think CABG, aorta, or mitral valve surgery.
Aortic Regurgitation
Aortic Regurgitation: Etiology
• Dilatation of aortic root & aortic annulus
-Ascending aortic aneurysm (Marfan’s, Ehlers Danlos,
bicuspid aortic valve, familial, annuloaortic ectasia,
ankylosing spondylitis, osteogenesis imperfecta)
-Chronic type A aortic dissection
-Arteritidies (Takayasu’s, giant cell, syphillis)
• Abnormal aortic valve cusps
-Calcific, bicuspid, rheumatic, radiation
-Endocarditis
-Anorexigens
-Prolapse (supracristal VSD)
�
Chronic Aortic Regurgitation:
Pathophysiology
• Diastolic leaking of blood back into LV leads to LV
volume overload
• LV compensates for volume overload by dilating
(eccentric hypertrophy)
• Stroke volume increases to maintain forward output
• Increased stroke volume leads to systolic hypertension
and pressure overload of LV
• LV compensates for pressure overload with concentric
hypertrophy
• With time eccentric hypertrophy fails and LV diastolic
pressure increases
• With time concentric hypertrophy fails and LV contractile
function falls ( EF declines)
� Aortic Regurgitation: Law of LaPlace
Wall Stress = Pressure x Radius
2x Thickness
39yamani02
�
Aortic Regurgitation:
Pathophysiology
48carabe04
655shaver001
�
Aortic Regurgitation:
Pathophysiology
97thomas179
�
Chronic Aortic Regurgitation:
Pathophysiology
655shaver010
�
Chronic Aortic Regurgitation:
Pathophysiology
655shaver011
�
Chronic Aortic Regurgitation:
Pathophysiology
655shaver012
�
Aortic Regurgitation: Presenting
Symptoms
• Forceful heart beat (especially recumbent)
• Angina
-Concurrent CAD
-Low aortic diastolic pressure
-LVH and increased muscle mass
• Congestive heart failure
-LV systolic dysfunction
-LVH and diastolic dysfunction
-Inability to augment cardiac output
�
Chronic Aortic Regurgitation:
Physical Exam
• Wide pulse pressure with elevated systolic
and low diastolic BP
• Manifestations of wide pulse pressure:
-Brisk/bounding carotid pulse (Corrigan’s pulse)
-Quincke’s pulse (pulsations in nailbeds)
-deMusset’s sign (head bobbing)
-Duroziez’s sign (systolic & diastolic bruits when femoral
artery lightly compressed)
-Traube’s sign (‘pistol shot’ sounds over femoral artery)
�
Chronic Aortic Regurgitation:
Physical Exam
• Soft S1
• Systolic ejection click if bicuspid aortic valve
• PMI displaced laterally and hyperdynamic
• S3 if LV systolic dysfunction has developed
• High pitched, decrescendo immediate diastolic murmur
-3rd left interspace (best leaning forward, held expiration)
-2nd right interspace if due to aortic root dilatation
-Intensity of murmur correlates poorly with severity of regurgitation
-Duration depends on chronicity & severity (longer in severe regurg)
• Early peaking systolic ejection murmur • Delayed diastolic, low-pitch apical murmur (Austin Flint)
� Chronic Aortic Regurgitation: Grading Severity
Mild Moderate Severe
Regurgitant Volume (ml) <30 30-59 >60
Regurgitant Fraction (%) <30 30-49 >50
Effective Regurgitant <0.10 0.10-0.29 >0.30
Orifice (cm2)
LV size Normal Mild Dilated
�
Aortic Regurgitation: Diagnosis
• Typical findings on physical exam
• Expected symtpoms
• ECG evidence of LVH, ST-T changes
• Echo/Doppler
-LV size & wall thickness
-LV systolic function
-Presence & severity of aortic regurgitation
-Aortic root dimension
• Contrast aortography • Invasive hemodynamics • Cardiac MRI
� Chronic Aortic Regurgitation: Natural History
graph
�
Chronic Aortic Regurgitation:
Natural History
• Asymptomatic with normal LV:
- Risk of death < 0.2%/yr
- Development of asymptomatic LV dysfunction 3.5%/yr
- Development of symptoms +/- LV dysfunction <6%/yr
• Asymptomatic with LV dysfunction:
- Progression to symptoms > 25%/yr
• Symptomatic:
- Mortality > 25%/yr
� Chronic Aortic Regurgitation: Therapy • AVR (+/- replacement of aortic root) • Vasodilator therapy (?)
-Patients with indication for surgery who are not
operative candidates
�
Chronic Aortic Regurgitation: Class I
Indications For AVR
• Severe, symptomatic aortic regurgitation
• Severe, asymptomatic regurgitation with
LV systolic dysfunction (EF <50%)
• Severe, asymptomatic regurgitation at the
time of CABG, aorta, or other valve
surgery
� Acute Aortic Regurgitation • Usually caused by endocarditis, type A aortic dissection, or trauma • LV has not had time to dilate, LV diastolic pressure increases dramatically • Forward cardiac output falls as a large amount of each stroke volume is lost backward • Results in pulmonary edema and cardiogenic shock • Classic findings of wide pulse pressure are NOT seen and diastolic murmur will be short • Requires emergent AVR
� A Case
67 yo woman referred for murmur which she has known about for a
‘few years.’ Over recent months she has noticed dyspnea climbing
stairs– before she was completely asymptomatic. On exam, BP
140/86. JVP appears normal. Carotid upstroke is mildly diminished
and delayed. Chest clear to auscultation. Cardiac exam with III/VI
systolic ejection murmur at RUSB radiating to carotids and apex
which is late peaking. No diastolic murmur is heard. The PMI is
sustained and a soft S4 is heard at the apex.
-Why is the carotid upstroke delayed and diminished ?
-What is the underlying valvular pathology and how severe is it ?
-What should be done about it ?
�
A Case Resolved
• The diminished and delayed carotid upstoke is
pulsus parvus et tardus and signifies severe
aortic stenosis
• The underlying valve lesion is aortic stenosis
and by exam it is severe (late peaking SEM,
pulsus parvus et tardus)
• As the patient is symptomatic, the appropriate
course of action is AVR (with pre-op coronary
angiography to evaluate for concurrent CAD)
�

