Pregnancy, parturition & lactation
From Iusmphysiology
- started here on 04/08/11.
[edit] Pregnancy, parturition, and lactation
[edit] Learning objectives
- Understand the processes of fertilization and implantation
- Understand the structure and function of the placenta
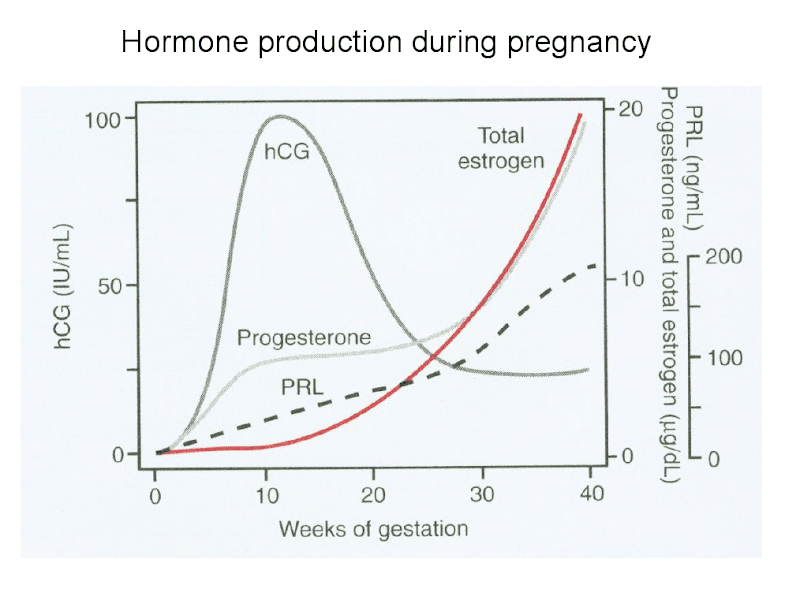
- Be familiar with the endocrine changes that occur during pregnancy
- Understand key concepts of parturition
- Understand key concepts of lactation
[edit] Pregnancy
[edit] Female anatomy review
- The female reproductive tract is composed of gonads that generate gametes and a series of ducts that maintain the gametes and the fetus.
- The gonads are the ovaries, found bilaterally and suspended from the posteriolateral wall of the abdomen by the ovarian ligaments.
- The beginning of the duct system is the fallopian tube (oviduct) which catches the evicted ocum via fimbria and passes it to the uterus via the ampulla and isthmus divisions.
- The uterus has a fundus, corpus, and cervix; the inside surface of the corpus is the endometrium which is the location of implantation and the connection point between mother and child during pregnancy.
- The cervix connects to the vagina.
[edit] Fertilization
- Fertilization is defined as the successful union of sperm and an egg.
- For fertilization to occur, both the egg and the sperm must be rapidly transported to their union because they each have a lifespan of only 2 days.
- Sperm transport through the female reproductive tract is best facilitated during the follicular phase; more to the point, sperm travels best through the female reproductive tract during the proliferative stage of the uterine cycle.
- Recall that the proliferative stage of the uterine cycle is characterized by endometrial hypertrophy and formation of spiral arteries.
- For proper fertilization, fresh sperm must be present as the ovum enters the oviduct (Fallopian tube).
[edit] Sperm transport
- About 250 million sperm are released upon ejaculation, however, only 50 million will make it to the oviduct.
- Loss of sperm is due to: acidic pH of the vagina, phagocytosis of sperm in the uterus, and the anatomical barrier presented by the uterotubal junction (that is, where the isthmus of the oviduct dumps into the uterus is a small opening that the sperm must find and proceed through).
- Sperm arrive at the oviduct in less than 5 minutes!
- That's about 0.5 sperm body lengths / second.
- Sperm are able to move through the female ducts because of their own motility and because of assisting vaginal, cervical, and uterine contractions.
- Semen initially coagulates (bad for transport) in the ducts and then liquefies (good for transport).
- During the follicular phase, mucin molecules of the cervical canal are oriented in parallel to facilitate transport of the sperm.
[edit] Capacitation
- Recall the basic anatomy of the sperm: three parts (head, middle, tail), an acrosome (sac of enzymes in the head), a nucleus, mt, and a tail (axoneme).
- Capacitation is a series of irreversible changes occurring in the sperm as a result of being delivered to the female reproductive ducts.
- Capacitation results in increased motility and happens after an hour of being delivered to the ducts.
- Changes during capacitation include: loss of surface proteins and lipids and merging of acrosome with cell membrane.
[edit] Ovum transport
- Recall that during ovulation, the oocyte of the dominant follicle is ejected from the ovary.
- Recall the basic anatomy of the follicle: many layers, theca x 2, granulosa, antrum, fluid, corposa oophorus, corona radiata, zona pellucida.
- The ejection of the egg leaves leaves the theca and granulosa layers to become the corpus luteum
- This makes sense when one recalls that the corpus luteum will go on to be the primary source of hormones and the granulosa cells and theca cells generate estrogen / progesterone and androgens, respectively.
- The ejected egg will therefore be composed of the cumulus oophorus, the zona pellucida, and the cell body of the oocyte.
- This oocyte is collected into the fallopian tube (oviduct) by way of ciliary action of the fibria.
- Some additional oocyte anatomy:
- The oocyte has three pre-cellular layers as it encouters sperm: the cumulus oophorus and corona radiata surrounding the zona pellucida.
- Deep to the zona pellucida is the perivitelline space that separates the zona pellucida and the oolemma (the cell membrane of the oocyte).
- The oocyte also has a series of microvilli just underneath the oolemma, which are poised to be an important part of the egg's interaction with sperm.
- Finally, recall that the first polar body will exist with the oocyte within the protective encasing of the cumulus oophorus, corona radiata, and zona pellucida.
[edit] Events of fertilization
- Fertilization takes place in the ampulla of the oviduct.
- Recall that 50 million sperm have made it to the oviduct and 1 egg has been moved into the oviduct via ciliary action of the fimbria.
- Recall that the sperm has undergone capacitation to make it a better swimmer and to merge its acrosome with the cell membrane at the tip of the head section.
- Recall that the egg that makes it to the oviduct is covered by the cumulus oophorus, the corona radiata, the zona pellucida, the perivitelline space, and the oolemma.
- The process of fertilization can be view as the solution to two major tasks: 1) getting through the layers surrounding the oocyte to the cell body and 2) keeping multiple sperm from fertilizing the oocyte.
- Getting through the protective layers of the oocyte:
- When the sperm and egg unite, the sperm breaks through the cumulus oophorus and the corona radiata to adheres to the zona pellucida of the egg.
- Adherence of the sperm to the zona pellucida is mediated by the ZP3 receptor.
- Adherence to the zona pellucida triggers release of the enzymes of the acrosome.
- Enzymes of the acrosome digest the cumulus oophorus.
I don't understand how binding the zona pellucida can cause release of enzymes that digest the cumulus oophorus when the oophorus is superficial to the zona pellucida.
- The sperm penetrate the zona pellucida in about 15-30 minutes.
- Once through the zona pellucida, sperm cross the perivitelline space (space between the zona pellucida and the cell membrane of the oocyte).
- Upon adhering to the oolemma (cell membrane of the oocyte), microvilli of the oocyte extend to grasp the sperm and the spermatic head and tail are engulfed.
Really? I think it has been shown that the tail is very specifically NOT engulfed.
- Keeping multiple sperm from fertilizing the oocyte:
- Once the oocyte has grasped the first sperm to penetrate the zona pellucida, the egg undergoes changes to the oolemma that prevent other sperm from entering the cell.
- Penetration of the first sperm through the oolemma causes Ca to enter the cell and two processes to begin: cortical granule release and the completion of meiosis 2.
- Rising Ca levels cause cortical granule fusion with the oolemma.
- As the cortical granules fuse the zona pellucida undergoes changes such that we call it the zona reaction, which is impermeable to sperm.
- As meiosis 2 completes, a single oocyte nucleus (1N) remains.
- Finally, a zygote is generated by the fusion of the male and female pronuclei.
What's the 2-3 degree about?
[edit] Twinning
- Twinning occurs in 3% of live births.
- There are two types of twinning: monozygotic and dizygotic.
- Monozygotic twinning occurs when one zygote splits into two separate, functional embryos and generates identical twins.
[edit] Fertilization to implantation
- The first mitotic division of the embryo occurs within 24-36 hours of fertilization.
- This initial cell division occurs in the oviduct, near the site of fertilization.
- Note that the embryo continues to be surrounded by the zona pellucida for the first several division generations for several reasons:
- transport, protection, and inhibition of immune reactions.
- As the fertilized egg travels along the oviduct it will undergo mitosis and form into a solid ball of cells called a morulla.
- The morulla enters the uterus approximately 4 days after fertilization.
Is this after ovulation or after fertilization?
- It is possible that an egg can become fertilized outside of the female reproductive tract resulting in an ectopic pregnancy.
- Ectopic pregnancies can be life-threatening if not treated.
[edit] Implantation
- The process of implantation is about physically attaching to the endometrium and establishing communication between the embryo and the mother's vascular system.
- A blastocyst implants in the endometrial wall of the uterus at approximately 7 days after fertilization and is fully embedded by 8-12 days post-ovulation.
- A blastocyst is a collection of 20-30 cells that have two distinct regions (the trophoblast and the embryoblast) with a fluid filled center.
- The trophoblast will go on to become all the extraembryonic tissue like the plaenta and umbilical cord.
- The embryoblast (inner cell mass) will go on to become the fetal tissue.
- The cells of the trophoblast commence the process of implantation by using proteases to invade the endometrium.
Is there a consistent location within the uterus for implantation? Does the location of the placental attachement change along the way? Does it effect parturition?
- The trophoblasts embedded in the endometrium differentiate into two cell populations to facilitate development of communication between the embryo and the mother's vascular system.
- Cytotrophoblasts: become villi and eventually chorionic villi.
- Syncytiotrophoblasts serve to increase the surface area for embryo-mother interaction and also secrete progesterone and hCG.
- Upon trophoblast invasion, the endometrium becomes undergoes changes to become a decidua in a process called the decidual reaction.
- The maintenance of the decidua requires progesterone from the luteal cells of the corpus luteum and the synciotrophoblasts.
- The decidua is characterized by large, polyhedral, multinucleated cells, dilated blood vessles, and lacunae.
- Eventually, the embryo will be composed of the three embryological tissue types: ectoderm, endoderm, and mesoderm.
[edit] Methods of contraception
- Pregnancy can be prevented at several points along the pathway of baby-generation: ovulation, fertilization, implantation.
- Preventing fertilization:
- Coitus interruptus is the removal of the penis from the female reproductive tract before ejaculation; coitus interruptus prevents fertilization by minimizing or preventing delivery of sperm to the female genital tract.
- The rhythm method of preventing fertilization relies on the timing of intercourse along the ovarian / uterine cycle. Since egg and sperm can only successfully fertilize during a several-day time frame (just after ovulation, before either cell degenerates), it is possible to time intercourse so that viable gametes do not come in contact.
- Barrier protection (like condoms) can inhibit the transfer of sperm to the female genital tract and thus inhibit fertilization.
- Preventing ovulation:
- Oral contraceptives provide estrogen to inhibit LH and FSH through negative feedback and thus inhibit development of the follicle.
Do oral contraceptives really "adversely affect the environment of the tract"?
- Morning after pill provides high levels of progestin or progestin and estrogen to ....
How does high levels of progestin / estrogen inhibit ovulation?
- Preventing implantation:
- IUDs contain a metal that irritates the uterine lining and prevents proper implantation microenvironment development.
- RU-486 provides long-acting progesterone, high doses of estrogen, or progesterone-receptor antagonists....
How does RU-486 work?
- High levels of prolactin (which can be maintained through regular breast-feeding) can suppress pulsatile release of GnRH and therefore prevent ovulation and pregnancy.
- Recall that GnRH from the hypothalamus stimulates LH / FSH release and that LH / FSH serve to mature the follicle and thus regulate ovulation.
- Note that one cannot assume that regular breast-feeding will prevent pregnancy.
[edit] Function of the placenta
- The whole point of the placenta is to exchange nutrients and waste, including:
- Oxygen / CO2 (via gradient, enhanced by HbF)
- Glucose, aa, electrolytes, hormones, etc.
- These are exchanged via diffusion, facilitated diffusion (non-energy dependent channels), and pinocytosis.
- Because the placenta effectively provides a blood-placental barrier, it can provide differential exchange.
What is differential exchange?
- It should be noted that not all drugs cross the placental barrier but most viruses do cross the barrier.
[edit] Structure of the placenta
- After implantation, the trophoblast offspring (cytotrophoblasts and synciotrophoblasts) interdigitate with endometrial cells to form chorionic villi and lobes called cotyledons.
- Recall that the placenta is designed to facilitate nutrient exchange between the mother and child.
- The placenta is said to be hemochoroidal because blood of the baby is brought to and from the villi (where it runs very near to the mother's blood) via two umbilical arteries and one umbilical vein.
- The fetal endothelium and connective tissue are bathed in mother's blood at the villi.
- The placenta has two layers: the aminon (inner-most) and the chorion (outer-most).
[edit] Endocrinology of pregnancy
- Make no mistake, the placenta is a temporary endocrine organ; the placenta produces several important hormones for the maintenance of pregnancy.
- The placenta produces progesterone, estrogen:
- Recall that estrogen and progesterone from the follicle and corpus luteum (follicular and luteal phases of the ovarian cycle) conditioned the female genital tract (uterus, cervix, vagina) for fertilization and implantation (the proliferative and secretory stages of the uterine cycle).
- So, it makes sense that the placenta would make progesterone and estrogen in order to maintain the microenvironment of the genital tract.
- The placenta produced human chorionic gonadotropin:
- hCG is produced by trophoblast cells of the placenta.
- hCG is an alpha-beta protein (alpha constant, beta unique) just like LH and FSH.
- hCG binds the LH receptors.
- Recall that the corpus luteum has granulosa cells and theca cells; recall, too, that theca cells have LH receptor throughout development of the follicle and granulosa cells begin to express LH receptor as the follicle matures to ovulation.
- Therefore, it makes sense that hCG is called a gonadotropin because hCG extends the life of the corpus luteum and elevates production of progesterone (by the reciprocal action of granulosa and theca cells).
- hCG peaks at 10-15 weeks.
- We suspect that hCG has a critical role throughout pregnancy.
- The placenta produces placental lactogen:
- hPL is produced by syncitiotrophoblasts of the placenta.
- hPL promotes milk-production (lactogenic) and somatic growth (growth-hormone-like).
- hPL ensures adequate fuel supplies for the
parasitefetus by reducing mother's glucose use and mobilizing mother's adipose reserves.
- The placenta produces other peptides:
What do I need to know about "other peptides"?
[edit] Steroid hormones of pregnancy
- The two major steroid hormones of pregnancy are progesterone and estrogen.
- Recall that progesterone and estrogen serve to condition the genital tract microenvironment for pregnancy.
- Progesterone:
- Produced for the first 8 weeks primarily by the corpus luteum.
- Recall that the trophoblasts of the placenta produce hCG which is a gonadotropin that maintains the life of the corpus luteum beyond the 2 weeks it would normally produce progesterone / estrogen while degrading during the luteal phase of the ovarian cycle.
- After 8 weeks, the trophoblasts of the placenta are the primary producers of progesterone.
- Trophoblasts have LDL receptors that collect LDL cholesterol from the mother's blood supply and convert it into progesterone.
- Progesterone levels rise throughout pregnancy.
- Progesterone conditions the genital tract in three ways: inhibits utrine contraction, inhibits prostaglanding formation, and inhibits immune response at the uterus.
- Specifically, progesterone binds to uterine smooth muscle cells to inhibit contraction.
- Specifically, progesterone inhibits T cell response at the uterus to provide temporary immune privilege to the uterus.
- Produced for the first 8 weeks primarily by the corpus luteum.
Why does it make sense that progesterone would inhibit prostaglandins? Would you want increased blood flow at the uterus?
- Estrogen / estradiol:
- Recall that estrogen is produced by the granulosa cells of the corpus luteum throughout the luteal phase (~2 weeks w/o pregnancy, extended to 8 weeks with hCG from placenta).
- Production of estrogens require a functional fetoplacental unit (that is, a functional connection between the fetus and the mother).
- Estrogen levels rise throughout pregnancy just like progesterone.
- Estrogen serves to condition the mother's genital tract: increases uterine size and increases uterine blood flow.
- Estrogen also affects fetal development; estrogen augments organ development and affects breast and adipose development.
- Lastly, estrogen is involved in implantation.
To what extent?
[edit] Maternal changes of pregnancy
- The physical presence of the growing fetus, along with estrogen, progesterone, and human placental lactogen cause changes to the mother's physiology.
- Recall that progesterone inhibits contractions, inhibits prostaglandins, and inhibits immune response at the uterus.
- Progesterone's inhibition of uterine contractions affects other smooth muscle, too, causing gastroesophageal reflux and constipation.
- Recall that the lower esophageal sphincter is smooth muslce (lower 1/3 is all smooth muscle) and the colon requires periodic smooth muscle peristalsis to move feces along so they do not dry out.
- Progesterone also causes increased minute ventilation.
- Progesterone's inhibition of uterine contractions affects other smooth muscle, too, causing gastroesophageal reflux and constipation.
- Recall that estrogen causes uterine growth and increased uterine blood flow.
- Estrogens cause increased blood flow systemically which can lead to sinus congestion, bleeding gums, and sensations of warmth.
- Estrogens cause increased perfomance of the cardiovascular system in general: increased blood volume, increased cardiac output, and increased heart rate.
- Recall that hPL (human placental lactogen from the synciotrophoblasts) causes milk production, reduced glucose use and increased adipose energy store mobilization in the mother.
- The mother will gain weight to ensure enough energy for fetal peak growth and in the case of starvation.
[edit] Endometriosis
- Recall that endometrial cells line the inside of the uterus and respond to estrogen and progesterone by proliferation.
- When endometrial cells exist outside of the uterus (like on the ovaries), they can proliferate and cause pathology.
- S&S include pelvic pain that worsens with the menstruation cycle.
- It makes sense that pain would increase during during the follicular uterine cycle and the luteal phase of the ovarian cycle because estrogen levels will be high.
- Endometriosis is in 5-10% of women--usually during the reproductive years.
- Endometriosis is a common cause of infertility.
[edit] Parturition
- Parturition is a poorly understood concept in general.
- We do know that there are both fetal and maternal factors that play a role.
- We know that there are both hormonal and mechanical factors.
- We suspect that paracrine factors may be the most important kind of hormone signaling involved in parturition.
- There are 5 major hormones that affect parturition: estrogen, progesterone, oxytocin, relaxin, placental-corticotropin releasing hormone (pCRH).
- We know that estrogen is generally pro-parturition and progesterone is generally anti-parturition.
- Estrogen's role in parturition:
- Recall estrogen is generally pro-parturition.
- Progesteron's role in parturition:
- Recall that progesterone is generally anti-parturition.
- In many species progesterone declines sharply just before parturition, however we don't know if progesterone decreases significantly in humans.
Is this the case?
- Recall that progesterone inhibits prostaglandins during pregnancy.
- During parturition, there is a sharp increase in prostaglandins in the amniotic fluid.
- So, we suspect that decreased progesterone during parturition allows increased prostaglandins.
- Increased amniotic prostaglandins stimulate contractions and cervical ripening.
- Recall that progesterone inhibits prostaglandins during pregnancy.
- Oxytocin's role in parturition:
- Oxytocin augments labor but doesn't increase uterine responsiveness or density (that is, it doesn't cause uterine contractions to be more forceful or more common).
- Recall that myometrial cells (uterine smooth muscle cells) can coordinate via gap junctions.
- Cervical and vaginal dilation causes explosive, pulsatile release of oxytocin during parturition.
- We believe that this release of oxytocin developed to help mother's deliver the subsequent litter-mates (and in humans the placenta).
- Note that women with a posterior pituitary defect proceed through parturition normally.
- Recall that the posterior pituitary releases oxytocin generated by the neurons of the nuerohyophysis.
- Oxytocin augments labor but doesn't increase uterine responsiveness or density (that is, it doesn't cause uterine contractions to be more forceful or more common).
- The role of relaxin is in parturition is unclear.
- pCRH's (placental corticotropin releasing hormone) role in parturition:
- pCRH (placental corticotropin releasing homrone) seems to affect the estrogen-progesterone ratio in sheep and humans.
- In general, pCRH increases exponentially near parturition.
- pCRH shifts production from progesterone to estrogen.
- This makes sense; recall that estrogen is pro-parturition and progesterone is anti-parturition.
- Recall that progesterone inhibits prostaglandins; so it makes sense that elevated pCRH is associated with elevated prostaglandins because pCRH causes a relative decrease in progesterone to estrogen.
- Additional evidence of the importance of pCRH:
- Sheep without anterior pituitary function or adrenal function (that is, lacking ACTH and cortisol) have longer gestation periods (that is, delayed parturition).
- Women who deliver early show elevated levels of pCRH within 24-48 before parturition.
[edit] Lactation
- Lactation is the production of milk by a woman.
- Lactation is primary controlled by the maternal pituitary gland.
- Recall that lactotropes (mammotropes) of the anterior pituitary produce prolactin.
- Recall that neurons of the neurohypophysis (posterior pituitary) produce and release oxytocin.
- Lactation requires suckling upon the nipple to be maintained; that is, neural sensation at the nipple is required for milk production by the mammary glands.
- Maternal milk is the "perfect nutrition source" for newborns because it is easy to digest, sterile, and the perfect temperature.
- Breast-milk infers several health advantages on the child: decreased risk of obesity, decreased ear infections, decreased food allergies, decreased GI illnesses
[edit] Development of the mammary glands
- Mammary gland precursor cells develop along the bilateral mammary ridges in both boys and girls.
- Accessory nipples can result from poor degenerative signaling that usually limits nipple development to just two, symmetrical nipples.
- There is an initial development and maturation of the mammary glands throughout fetal and post-natal development.
- This initial development is identical in boys and girls and allows the glands to be responsive to hormonal signals.
- Note that this development stage sets the mammary glands up to either be signaled to develop further by the relatively high estrogen levels pregnancy or to remain under-developed in boys.
- Secondary development is characterized by the change of connective tissue to milk ducts and occurs in response to hormone elevation during pregnancy.
What is witch's milk in newborns?
[edit] Anatomy of the breast
- Breast tissue contains epithelial milk producing cells arranged in alveola, myoepithelial cells surrounding the alveoli, and epithelial lined tracts.
- Cuboidal epithelial cells that make up the alveoli are signaled by prolactin to produce milk and secrete it into the epithelial secretory alveoli (the beginning of the ductule system).
- Myoepithelial cells around the alveoli are signaled by oxytocin to contract, thus squeezing milk along the tracts.
- The epithelial ductule system of mammary glands begins as the tract within alveoli called secretory alveoli, progresses to intralobular ducts, and then to collecting ducts that converge on the nipple.
[edit] Characteristics of human milk
- The characterisitics of human milk change over a short time frame post-parturition.
- The initial milk produced is called colostrum and is high in lymphocytes and antibodies which is good for helping the baby deal with its new, infectious environment.
- The milk matures from colostrum into hindmilk within three days.
- Hindmilk contains higher fat content which promotes satiety in the newborn.
- Note that pregnancy and lactogenesis are well coordinated because lactogenesis occurring with pre-term delivery generates milk with a higher protein and fat concentration which makes sense because the newborn has some extra growing to do.
[edit] Lactogenesis
- Milk production begins in the 5th (~20 weeks) month of gestation.
- Note that only colostrum is produced before and immediately following parturition.
- Production of hindmilk is inhibited by high progesterone and estrogen levels of pregnancy.
- Recall that estrogen and progesterone are produced by the placenta so it is not until the placental source is arrested (via parturition) that hindmilk can be produced.
- Progesterone and estrogen are prolactin antagonists.
[edit] Role of prolactin
- Recall that prolactin is produced by lactotrophs of the anterior pituitary.
- Estrogen increases prolactin production during pregnancy. (Recall that estrogen levels rise throughout pregnancy and that estrogen is a prolactin antagonist).
- Note that estrogen increases prolactin levels but decreases prolactin's ability to have an effect at the mammary gland tissue.
- Recall that dopamine is constantly expressed in non-pregnant females to inhibit prolactin production at the anterior pituitary.
- Estrogen increases prolactin production during pregnancy. (Recall that estrogen levels rise throughout pregnancy and that estrogen is a prolactin antagonist).
- Prolactin has several effects at the mammary tissue: increases milk production, stimulates lactose production, and stimulates expression of milk-protein genes.
- Prolactin production increases at each nursing (that is, it is produced as a result of suckling stimulation).
[edit] Role of suckling
- An infant suckles on the nipple in a back-to-front action.
- Stimulation at the nipple by an infant has a short term and a long term effect via neuronal-hormonal reflex arcs: milk secretion and milk production.
{The infant does not suckle "on the nipple". To stimulate Prolactin the infant must be deeply attached to the breast with breast tissue filling the cheeks.}
- The afferent (at the CNS) signal for these reflex arcs is physical stimulation of the neurons that innervate the nipple.
- The short term, milk-secretion arc occurs through neuronal secretion of oxytocin (the hormonal efferent--exit the CNS signal) from the neurohypophysis (posterior pituitary) which stimulates the myoepithelial cells surrounding the mammary gland alveoli to contract, secreting milk for the infant.
- The long term, milk-production arc occurs through increased prolactin production (the hormonal efferent--exit the CNS signal) which causes increased milk production by signalling the epithelial cells of the mammary gland alveoli.
- Milk-let down is the release of milk from the lactiferous ducts to the lactiferous sinus.
{Lactiferous sinuses have been disproven. You are using outdated information}
- The let down effect may be secondary to CNS effects (meaning stimulation at the nipple gets to the posterior pituitary via the CNS and causes oxytocin release).
[edit] Role of oxytocin
- Oxytocin has social-behavioral effects in addition to the direct physical effects previously described (think myoepithelial signaling, milk-secretion, dilation of cervix and vagina).
- Indeed, oxytocin has been considered a love potion.
- Oxytocin acts as a nuerotransmitter in the brain and is associated with maternal nurturing behavior, trust, decreased fear, increased empathy.
- Oxytocin is also associated with female orgasm and a habit of long-term mating.
[edit] Sustaining lactation
- Lactation can be maintained for years after parturition given regular stimulation of the nipple.
- The supply of milk produced by the mother is determined by the need of the baby.
- Maximum volume production falls within 800-1200 ml / day.
- High levels of prolactin (which can be maintained through regular breast-feeding) can suppress pulsatile release of GnRH and therefore prevent ovulation and pregnancy.
- Recall that GnRH from the hypothalamus stimulates LH / FSH release and that LH / FSH serve to mature the follicle and thus regulate ovulation.
- Note that one cannot assume that regular breast-feeding will prevent pregnancy.
[edit] Summary
- Steroid hormones of pregnancy produced with maternal, fetal and placental contributions
Where did we see fetal contribution?
- Human parturition poorly understood
- Lactation involves hormonal regulation as well as neural response to infant suckling
- stopped here on 04/07/11.
