Male reproductive physiology
From Iusmphysiology
- started here on 04/06/11.
[edit] Male reproductive physiology
[edit] Learning objectives
- Recognize the structure and functions of the male reproduction organs
- Understand the process of spermatogenesis
- Understand steroidogenesis
- Understand disorders of male reproduction
[edit] Anatomy
- The creamaster muscle and the pampiniform plexus help regulate the temperature of the testes.
- The cremasteric muscle can pull the testes up toward the abdomen for increased heat.
- The pampiniform plexus of vessels provides lots of blood flow and lots of heat.
How much more anatomy do I need to know from this slide?
[edit] Characteristics of the testes
- The testes have two functions: spermatogenesis and steroidogenesis.
- The seminiferous tubules are the site of spermatogenesis.
- The seminiferous tubules are very small tubules that radiate through the testicle from the rete testis.
- Two cell populations comprise the seminiferous tubule: germ cells and Sertoli cells.
- Germ cells generate new sperm.
- Sertoli cells play a supporting role to germ cells.
- Leydig cells produce testosterone.
- Leydig cells are also called "interstitial cells of the testes" because they reside between the seminiferous tubules.

- Note the epididymis, seminiferous tubules, lobules, and vas deferens.
[edit] Structural organization of the testes
- The cellular organization within the seminiferous tubules is focused on generating a blood-testes barrier.
- The blood-testes barrier is important to prevent immunological attack upon the developing sperm.
- To form this barrier, sertoli cell surround the germ cells that generate sperm.
- Sertoli cells span the entire width of the seminiferous tubule.
- There are two compartments in the seminiferous tubules: basal and adluminal compartments.
- The basal compartment contains the least mature sperm and is nearest the border of the tubule.
- The adluminal compartment contains the most mature sperm and is in the center of the tubule.


[edit] Sertoli cell supportive functions
- Recall that sertoli cells are supportive cells to germ cells.
- Sertoli cells are important for spermatogenesis in three ways: phagocytizing defunct germ cells, spermiation, synthesis of transferrin.
- Spermiation: "the release of the spermatozoon from the seminal epithelium into the lumen of the seminiferous tubule." per academia
- Sertoli cells provide plasmin, an enzyme that causes release of spermatozoa from the epithelium of the seminiferous tubule into the lumen.
- Recall that spermatozoa are fully mature male gametes.
- Note that transferring is important for spermatogenesis.
[edit] Sertoli cell secretory functions
- Sertoli cells have g-protein FSH receptors that drive cAMP and PKA.
- cAMP and PKA in sertoli cells have several effects, all of which generally lead to increased signaling and proliferation.
- Increased release of androgen binding protein.
- Recall that ABP carries testosterone and DHT in the blood.
- Increased release of inhibin.
- Recall that inhibin inhibits the pituitary (FSH / LH).
- Induction of P450 aromatase
- Recall that P450 aromatase converts testosterone to estradiol.
- Increased release of plasminogen activator
- Recall that plasminogen activator is a serine protease that breaks down clots.
- Increased cell proliferation
- Increased release of androgen binding protein.
[edit] Sertoli cell products
- Sertoli cells proudce three major products: ABP, Inhibin, Plasminogen activator
- Androgen binding protein:
- 90Kd, heavy and light chain
- Binds Test and DHT with high affinity
- Used for carrying androgens in the Sertoli cells and epididymis.
- Used for storing androgens in the seminiferous tubule
- Inhibit
- Provides negative feedback to the pit.
- Plasminogen activator
- Cuts plasminogen into plasmin which goes on to digest fibrin (a key structural protein in clotting).
[edit] Leydig cells
- Recall that leydig cells reside in the interstitium, between seminiferous tubules.
- Know this, it kind of makes sense that leydig cells are derived from mesenchymal cells as they are sitting in a connective tissue area.
- Leydig cells are especially focused around blood vessels.
- Leydig cells are primarily a reservoir of lipids that can be used to generate testosterone.
- Leydig cells appear foamy because of the presence of secondary lipid droplets.
- The lipid droplets are esterified cholesterols which can be used for testosterone production.
- Testosterone production requires two major steps and three locations:
- The first major step occurs in the cytoplasm: hydrolyzing the esterified cholesterol into free cholesterol.
- The second major step occurs in the mitochondria: converting cholesterol into pregnenolone.
- Note that chol->pregnenolone is the rate-limiting step.
- The third location is the endoplasmic reticulum where testosterone is finally generated.
[edit] Leydig actions
- Leydig cells have LH receptors that stimulate release of testosterone.
- Sertoli cells and Leydig cells demonstrate reciprocal hormonal communication.
- As the Leydig cells release testosterone (via LH signaling), the Sertoli cells use their P450 aromatase to convert it to estradiole (E2) and send it back to the Leydig cells.
- The function of E2 (estradiol) signaling on Leydig cells is unclear.
[edit] Additional products of the testes
- The testes also make several other products:
- Opiods
- AVP
- Oxytocin
- GnRH-like peptide
- Growth factors
- Neurotransmitters
Anything more to know from this slide?
[edit] Spermatogenesis
- Spermatogenesis is a well scheduled event so there are phases and cycles.
- The three phases are: mitosis, meiosis, and spermiogenesis
- Cycles last 65-70 days and new cycles begin every 2-3 weeks.
[edit] Germ cell mitosis and meiosis
- The cells of spermatogenesis proceed in a particularly named order through a series of specific types of divisions:
- Cell (count): primordial germ cell (1) -> spermatogonia (1) -> primary spermatocyte (32) -> secondary spermatocyte (64) -> spermatids (64) -> spermatozoa (64)
- Note that primordial germ cells, spermatogonia, and primary spermatocytes are diploid whereas secondary spermatocytes, spermatids, and spermatozoa are haploid.
- Divisions: Mitosis -> meiosis 1 -> meiosis 2.



[edit] Spermiogenesis
- Spermiogenesis (as opposed to spermatogenesis) is the specialization of the spermatid into the spermatozoa.
- Four major changes take place to form a highly specialized cell:
- Nearly all the cytoplasm is lost.
- Nuclear chromatin is condensed and altered.
- The axoneme (tail) is formed: centrioles rearrange and relocated to form a 9x2 arrangement on the cell membrane.
- the axoneme has a fibrous sheath, too.
- The acrosome is foromed: a collection of enzymes surrounds the nucleus at the opposite pole as the tail.
- There are three major sections to the completed spermatozoa:
- The head, made of the acrosome (collection of enzymes).
- The middle, made of spiral sheathes of mitochondria for energy.
- The tail--also called the axoneme--propels the cell forward by a twisting motion.
[edit] The axoneme
- Recall that the axoneme is generated from the spermatid's centriole.
- There is an intricate structure to the axoneme that is important for its function.
- At the center is the central tubule with 2 tubules.
- Radiating from the outside toward the center are the radial spokes.
- Radial spokes are connected to the exterior structure by Y links.
- Radial spokes are connected to adjacent radial spokes by bridges.
- Along the radial spokes are 9 sets of doublet tubules.
- The axoneme uses dyenein motors on the doublet tubules to generate a spiral twisting which generates movement.
[edit] Role of testosterone and FSH in spermatogenesis
- Both FSH and testosterone are required for spermatogenesis.
- Recall that Sertoli cells have receptors for both FSH and testosterone.
- Recall that testosterone is generally coming from the Leydig cells because of LH signaling.
- Recall that FSH is coming from the anterior pituitary.
- While FSH is required for initiation of spermatogenesis, testosterone is sufficient to maintain progressing spermatogenesis.
- Testosterone is required for capacitation: the process that allows spermatozoa to generate motion and occurs in the epididymis.
[edit] Seminal fluid
- Seminal fluid (semen) is the entire combination of fluids ejaculated.
- Seminal fluid contains:
- 10% sperm by volume
- seminal vesicle fluid: 75% by volume
- prostatic secretions
- bulbourethral secretions
- Seminal fluid has fructose (nutrient for spermatozoa), ascorbic acid (I think has something to do with maintaining pH once in the female UG tract), prostaglandins (increase blood flow), and fibrinolysin (cut up clots).
[edit] Expulsion of semen
- Semen expulsion is a neuromuscular reflex with two phases: emission and ejaculation.
- Emission moves sperm and the rest of the seminal fluid contributions into the urethra.
- The lumbar spine nerves control the muscular contractions of the epididymis and vas deferens.
- Ejaculation moves semen out of the urethra.
- Ejaculation requires a second spinal reflex and contraction of the bulbospongiosus muscles that surround the uretra.
- Recall from anatomy that Pointing and Shooting require Parasympathetics and Sympathetics, respectively.
[edit] Testicular steroidogenesis
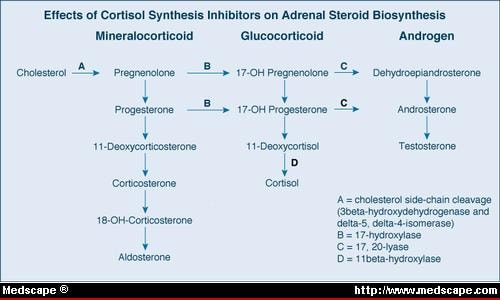
- Recall the hormone synthesis pathway of the adrenal gland:
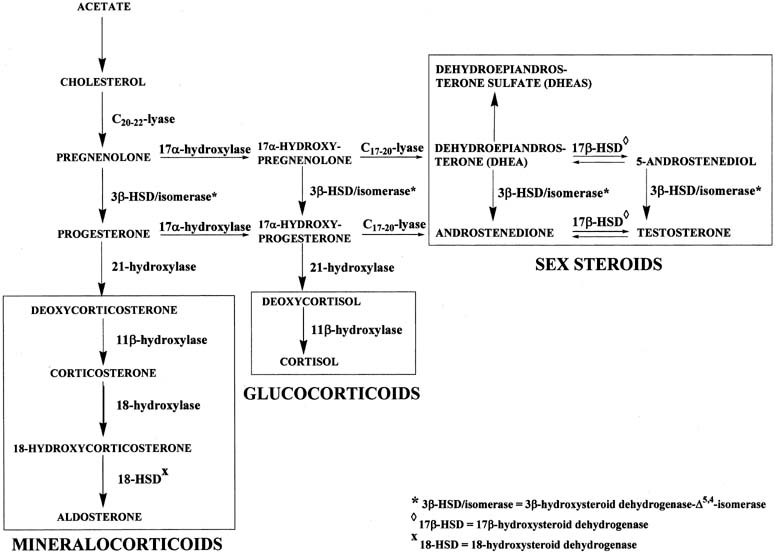
- Which of these end products is produced is determined by the predominant enzyme present.
- By genetic determination of the predominant enzyme expressed, tissues like the testes, the adrenal glands, and the ovaries can become functionally specific.
- In the testes, testosterone is the primary product generated.
- Pregnenolone is the key intermediate for the testes.
- Note that delta 5 or delta 4 can be used along the pregnenolone -> testosterone pathway.
[edit] The LH receptor
- Recall that the Leydig cells contain cholesterol stores and generate testosterone upon LH signaling.
- Leydig cells have 15K LH receptors / cell yet less than 5% need to be activated to generate a response.
- This means that Leydig cells can detect very low levels of LH.
- The LH receptor signals through a g-protein coupled receptor, cAMP, and PKA.
- Ultimately, testosterone is generated and released.
[edit] Familial male precocious puberty (FMPP)
- Familial male precocious puberty (FMPP) is also called testotoxicosis.
- Testotoxicosis is "familial" because a mutation of the LH receptor can cause this disease.
- Mutations of the LH receptor have been shown to cause excessive inactivation (and thus excessive and early release of testosterone and thus precocious puberty).
- At least 15 mutations have been identified.
- Most mutations involve ASP478.
- Clinical manifestations of FMPP include:
- precocious puberty by age 2-6
- secondary sexual development
- acne
- growth acceleration and advanced skeletal maturation
- behavior problems
- Note that female carriers of the mutated LH receptor are unaffected.
- Treatment of FMPP:
- Apply an androgen receptor blocker to inhibit the excessive and early testosterone.
- Apply an aromatase inhibitor lest the testosterones get aromatized into estrogen (via Sertoli cells as one example).
[edit] Metabolism of testosterone
- Recall that testosterone is generated by Leydig cells upon LH signaling.
- Testosterone is a steroid so it can immediately diffuse out of the producing cell into the blood.
- In the blood, most testosterone (97-98%) is bound to carrier proteins (steroid hormone binding globulin, SHBG).
- SHBG acts as a reservoir for testosterone.
- SHBG is increased by estradiol signaling on the liver.
- Plasma testosterone is generally converted to DHT or E2 (estradiol) at the target tissue:
- DHT: prostate, scrotum, penis, bone
- E2: fat, liver, CNS, skin, hair
- 17 ketosteroid: liver, kidney
- Test: testes, pituitary, muscle
- Conjugate: liver, kidney
[edit] DHT, dihydrotestosterone
- DHT is two to three times more potent than testosterone.
- DHT is critical for normal sexual differentiation.
- 5-alpha reductase converts testosterone to dihydrotestosterone (DHT).
- 5-alpha reductase is also active in hair follicles and sebaceous glands.
[edit] Estradiol
- Estradiol is generated by many tissues (including testes and the brain) from testosterone.
- Abnormal levels of E2 causes gynecomastia (breast enlargement).
*E2 levels in men rise nearly to those of women when the man goes through the follicular phase. Does he really mean this?
[edit] Actions of androgens
- Androgens have affects on physical differentiation, brain masculinization, and physiological properties.
- Physical differentiation: sexual differentiation (see Sexual differentiation, HPG axis), secondary sexual characteristic development (hair, acne, voice, growth), hair growth (and balding).
- Physiological properties: lipid levels, RBC mass
- Masculinization of the brain
- There are many androgen receptors on the brain.
- Although we know that hierarchy and copulating patterns in animals are correlated with androgens, there is no correlation between libido and androgen levels in human males.
- Females exposed to excess androgens during development (in utero) demonstrate increased "male typical" behavior.
[edit] Worldwide trends in male reproductive function
- We are currently observing trends that make us think reproductive function may be declining:
- serum testosterone levels are decreasing in the US and Europe.
- Sperm concentration has decreased by nearly half over the past 70 years.
- Semen quality differs geographically and has been shown to correlate with pesticide expsoure (less semen production upon exposure).
- There is an increased incidence of cryptorchidism, hypospadias, and testicular cancer.
- Cryptorchidism: "a condition seen in newborns whereby one or both of the male testes has not passed down into the scrotal sac." per Driscoll Chidlrens
- Hypospadias: "an abnormal condition in males in which the urethra opens on the under surface of the penis" per Princeton's wordnetweb
[edit] Disorders of male reproduction
- Half of the infertility of men is caused by endocrine disorders.
- Hypothalamic-pituitary hypogonadism results from a defect in the HPG axis: Kallman syndrome, GPR54 gene mutations, and GnRH receptor mutations.
- Recall that GPR54 receptor mutations lead to decreased GnRH release by the neurons of the hypothalamus upon kisspeptin signaling.
- Recall that GnRH receptor mutations lead to decreased LH / FSH release by the gonadotrophs in the anterior pituitary upon GnRH signaling from the hypothalamus.
- 'Primary hypogonadism occurs because of defects in the gonads: Klinefelter syndrome, testicular regression, acquired hypogonadism
- Recall that Klinefelter syndrome results from a 47XXY karyotype that causes underdeveloped testes and therefore decreased testosterone levels.
- Note that testicular regression syndrome covers "a variety of conditions in which both testes regress during fetal life. It is also known as pure gonadal dysgenesis, Sawyer's syndrome, true agonadism, testicular dysgenesis, vanishing testis and complete bilateral anorchia" per Medcyclopaedia.
- Recall that "true" gonadal dysgenesis resulted from a defect in the SRY region.
- Acquired hypogonadism can occur because of infection or abuse of anabolic steroids.
- Other endocrinopathies: hyperprolactinemia, excess androgens
[edit] Kallman syndrome
- Kallman syndrome results from the mutation of the cell adhesion gene KAL.
- KAL is ubiquitously expressed in all tissues of the body and even escapes X inactivation.
- KAL is located on the p arm of the X chromosome.
- The KAL gene generates anosmin as a protein product; anosmin is an important component of the basement membrane.
- When KAL is mutated in XY males, hypogonadotropic hypogonadims and anosmia results.
- Without functiona anosmin, GnRH secreting neurons of the olfactory placode fail to migrate to the medial basal hypothalamus (MBH).
- Improper migration leads to olfactory bulb dysgenesis and decreased GnRH release:
- In some cases, the pt cannot smell
- In most cases, the pt has poor gonad development, poor secondary sexual characteristic development, and poor puberty development.
[edit] Conclusions
- Testes produce both steroids and sperm.
- Spermatozoa are the end product of spermatogenesis and are highly specialized cells.
- Androgens affect physical appearance, the brain, and physiology.
- Disorders of male reproduction can result from endocrine and non-endocrine (Kallman Syndrome) etiologies.
- stopped here on 04/07/11.