Dermatology - Pediatric Birthmarks and Exanthems
From Iusmicm
Contents |
[edit] Pediatric Birthmarks and Exanthems
[edit] Objectives
- Differentiate common pediatric birthmarks
- Understand the natural history and treatment options
- Be familiar with signs and symptoms associated with various pediatric exanthems
[edit] Pediatric Birthmarks
- There are three major types of pediatric birthmarks: hemangiomas, port-wine stains, and congenital melanoytic nevi
- An exanthem is a cutaneous lesion whereas an enanthem is a mucous membrane lesion.
[edit] Tumors versus Malformations
- We classify birthmarks as either tumors or malformations, depending on the amount of abnormality of the structure
- Tumors include (proliferative): infantile hemangiomas, tufted angiomas, and kaposiform hemangioendotheliumas
- Malformations include (abnormal formation): port-wine stains (capillary), venous, lymphatic, and arteriovenous malformations
[edit] Infantile Hemangiomas
- An infantile hemangioma is a benign tumor of vascular endothelium
- About 4-5% of Caucasian infants develop an infantile hemangiomas
- Most hemangiomas develop in the first year of life
- Most spontaneously regress by age 5-10
- http://3.bp.blogspot.com/_uH5esL2gOT0/SFfBjYtEOLI/AAAAAAAAAuI/_YE8XMRxYSo/s400/hemangioma
- Risk factors include: being female, premature birth, low birth weight, and being a twin
- We no longer use the terms "capillary" or "cavernous" when describing hermangiomas (in an attempt to standardize the nomenclature).
- Infantile hermangiomas can be superficial, deep, or mixed.
- Infantile hermangiomas can be localized, segmental, indeterminate, or multifocal.
- Ulceration is one of the complications when hemangiomas are at a high-friction area.
- Localized:
- Doesn't indicate underlying structural development issues


- Segmental:
- Often associated with improper development of a particular metamome (embryological unit)
- May indicate underlying structural developmental issues




- Indeterminate:
- Multifocal:
- Treatment for infantile hermangiomas
- Observation (90% or more)
- Corticosteroids (for large, disfiguring, ulcerating, etc.)
- The mainline therapy
- Likely works by inhibiting factors that promote angiogenesis
- Beta-blockers: propranolol, timolol
- An alternative therapy
- Likely works by inhibiting VEGF / FGF, inducing vasoconstriction, and perhaps even by inducing apoptosis of the endothelial cells
- Based on case studies as of now
- Interferon-alpha
- An alternative therapy
- Used when corticosteroid are not effective
- A potent inhibitor of angiogenesis
- Laser therapy (selected cases)
- Only after involuted if it leave some tissue behind.
- Cannot be used on the primary hemangioma
- Surgical excision (rarely)
- Vincristine
- An alternative therapy
- A mitotic inhibitor from madigascar periwinkle that is used as a chemotherapy
- Induces apoptosis of tumor cells and endothelial cells
- Also used in other infantile birthmark tumors like tufted angiomas and kaposiform hemangioendotheliomas
[edit] Capillary malformations
- Capillary malformations cause vascular stains on the superficial epdiermis.
- These are often colloquially referred to as as a "salmon patch", an "angel's kiss", a "stork bite", or a "nevus simplex"
- May light up upon normal physiological capillary dilation (anger, hard work, etc.)
- Capillary malformations are very common
- Capillary malformations tend to occur on the glabella, the eyelids, the nose, the upper lip, and the nape of the neck.
- Note that the glabella is the smooth part of the forehead above and between the eyes
- Most capillary formations fade over 1-2 years, except those in the neck location.
- Capillary malformations include many types; we will focus on port-wine stains.

[edit] Port-wine stain
- A port-wine stain is a superficial vascular malformation
- Less than 0.5% of live births manifest a port-wine stain
- Port-wine stains do not regress
- Can generate capillary malformations that can bleed.
- There is potential for a port-wine stain to thicken and develop benign vascular papules
- Recall that a papule is a "Circumcised, flat (non-palpable), discolored".
- A macule is a small papule.
- Treatment for port-wine stain is by vascular lasering
- Lasers selectively destroy certain cells while leaving surrounding cells intact
- In this case we aim for the vascular cells but not the rest of the dermal / epidermal cells
- Port-wine stains can be progressive: darkening, developing blebs, developing bone and soft tissue hypertrophy
- Describe PW stains by their trigeminal distribution
- Because in V1 or peri-optical, we worry about WEb-Sturger syndrome with neuro issues
- Should be monitored regularly
- Because in V1 or peri-optical, we worry about WEb-Sturger syndrome with neuro issues
[edit] Port-wine stains and Sturge-Weber Syndrome
- Sturge-Weber syndrome is characterized by:
- Port-wine stains, seizures, mental deficiency, intracranial bleeding, intraocular bleeding
- Sturge-Weber sydndrome is only associated with port-wine stains in the CN5 V1 distribution
- 15% of V1 PWS will end up with Sturg-Weber syndrome
- Bilateral V1 port-wine stains are at higher risk for having Sturge-Weber syndrome
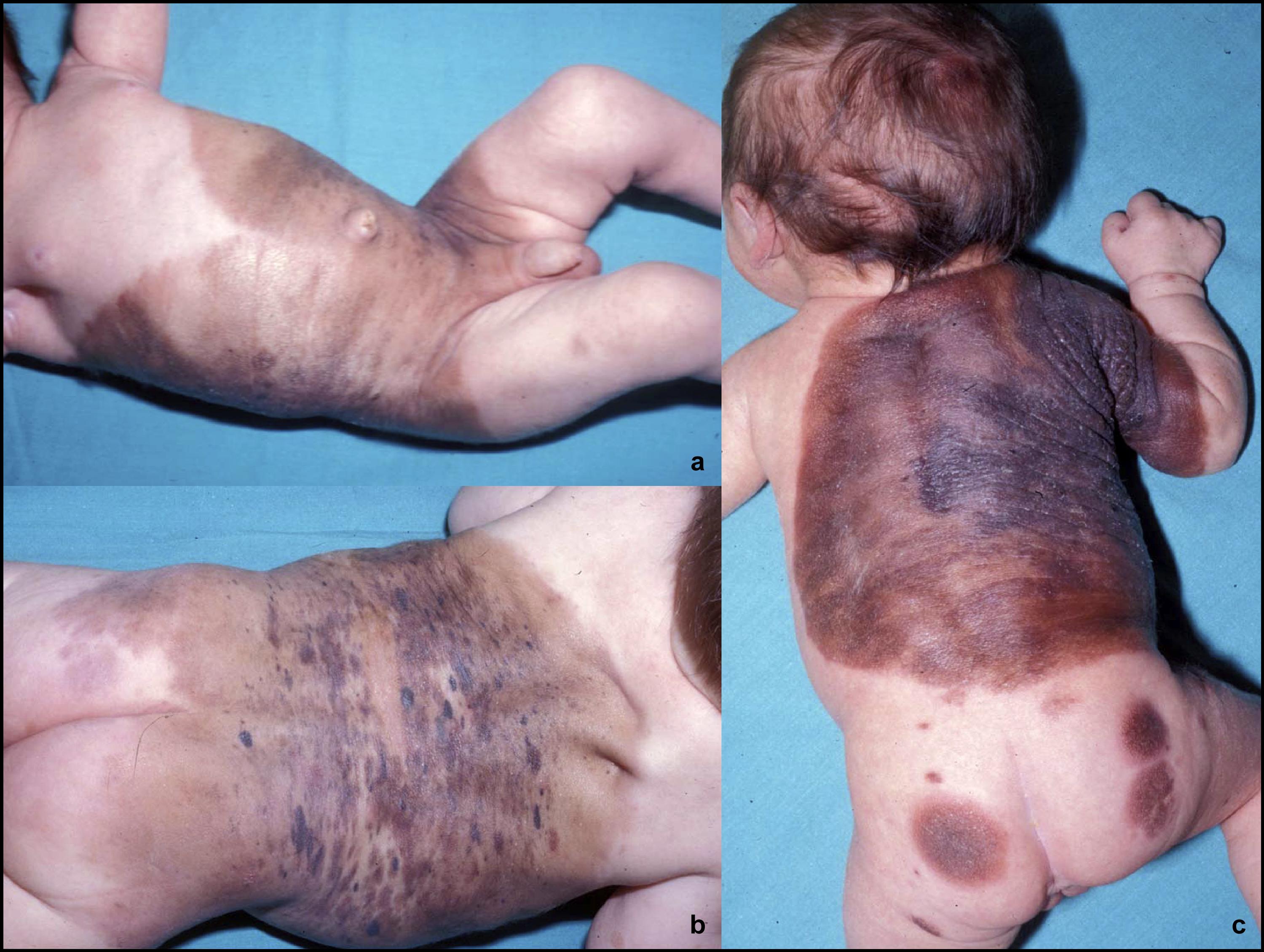
[edit] Congenital Melanocytic Nevi
- Another form of infantile birthmark is the melanocytic nevi
- Melanocytic nevi are bening hamartomas of melanocytic cells
- Recall that a hamartoma is an abnormal growth of normal cells
- We classify melanocytic nevi by their size: small, medium, and large.
- Size < 2cm
- Medium is less than 10-20 cm
- Large is bathing-trunk size
- 20% risk for melanoma
- 50% of melanomas develop in the first 5 years
- CMN (congenital melanocytic nevus) management includes monitorying and potentially surgical removal
- Watch for the ABCDEs (asymmetr, irregular borders, heterogenous color, large diameter, and expansion)
- May remove only small, hard to follow areas of really large nevi

- CMN may develop a nodule or other characteristics whereas acquired nevi are unlikely to develop secondary characteristics.
[edit] Childhood Exanthems
- An exanthem is an eruption at the skin secondary to a system infection.
- Examples of systemic infections that cause exanthems:
- varicella (chickenpox),
- rubeola (measles),
- rubella (German measles),
- roseola infantum,
- erythema infectiosum,
- hand-foot-mouth disease,
- scarlet fever
[edit] Varicella (Herpes = Chickenpox)
- Varicella is a systemic infection by herpes
- VZV = varicella zoster vaccine
- Can result in systemic infection; rare
- Usually occurs in immune deficient pts
- One type is zn deficiency
- Incubation of the infection takes 14-16 days
- Characterized by itchy lesions at different stages
- Described as "dew drops on a rose petal"
- It is better to get chickenpox as a child!
- Because older pts are more likely to have pulmonary complications via varicella pneumonia.
- Clinical vignette: 3 yo male presents with fever, headache, sore throat. Develops a rash on face several days later. Facial rash is followed by papular (as in a large, circumscribed, non-elevated, discolored patch) rash on face and over trunk and extremities including the palms and soles. Palpetral conjunctivitis and photophobia followed.
- Recall that a Tsanck smear is used to diagnose chickenpox / shingles
[edit] Rubeola (Measles, Morbilli)
- Morbiliform means measles; anything can be the cause, but it is showing up like measles
- Rubeola (measles) is a systemic infection by a paramyxovirus of the genus Morbillivirus
- Rubeola has a 10-14 day incubation period
- Recall that varicella's incubation period is 14-16 days
- Rubeola (measles) presents as cough, coryza, conjunctivitis, photophobia, and fever.
- Coryza is catarrhal inflammation of the nasal mucuc membrane
- Catarrhal is having to do with a respiratory infection
- Rash begins on day 4-5; morbilliform eruption
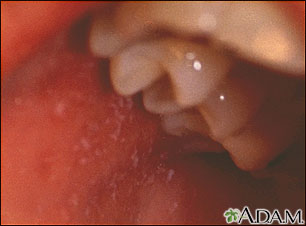
- Rubeola (measles) is characterized by koplik spots on the oral mucosa
- Small, irregular, bright red spots with a central bluish-white speck
- Usually near the second molars
- Appear 24-48 hours before the rash
- Complications of Rubeola:
- Bronchitis
- Encephalitis (1 / 1000)
- Ear infection (otitis media)
- Pneumonia
- Measles (rubeola) was eradicated in the US in 2000
- There are still 30-40 million deaths worldwide each year
- In the US in 2011, there have been 211 cases so far
- 25 of them are in California
- 85% of them are in unvaccinated children
- Vaccination exemptions are on the rise
- CDC predicts that an outbreak can occur if 5-10% of the population is not vaccinated
- Measles (rubeola) clinical vignette: a 4 yo boy has a low grade temperature, sore throat, cough, and lympadenopathy followed by a rash on the face that spreads to the trunk and extermities. Eruptiosn disappear 2 days later but a mild desquamation resides
- Note that both varicella and rubeola have a rash that starts on the head and moves to the trunk / extremities.
- Varicella has a fever, photophobia, conjunctivitis, and rash on the palms and soles that set it apart from rubeola.
- Rubeola has lymphadenopathy and eruptions that resolve in 48 hours, which sets it apart from varicella.
[edit] Rubella (German Measles)
- Rubella is a systemic infection by rubella virus
- A morbilliform illness
- Rubella (German Measles) is considered a milder form of rubeola (measles)
- Rubella (German Measles) has a 14-21 day incubation
- This is a longer incubation period than varicell (14-16 days) and rubeola (10-14 days)
- Rubella is characterized by encephalitis and thrombocytopenia (which set it apart from rubeola)
- Rubella has a progression twoard the cephalocaudal poles.
[edit] Erythema Infectiosum (fifth disease)
- Erythema infectiosum is a systemic infection by parvovirus B19
- Can recur in just a couple weeks
- Note that "fifth disease" was a name given in recognition that erythema infectiosum was typically the fifth sickness a child experienced.
- Incubation is 7-14 days
- Potentially shorter than varicella, rubeola, and rubella
- Erythema infectiosum has three distinct phases: slapped cheeks, fishnet erythema, and recurrence
- Erythema infectiosum is marked by purpuric (itchy) petechiae-like lesions in a gloves and socks distribution.
- Erythema infectiosum clinical vignette: 2 yo active child has 4 days of fever (up to 102F); parents no other symptoms. On 5th day, fever resolves and full body non-pruritic rash is observed.
[edit] Roseola Infantum
- Roseola infantum is a infection by herpes, strains 6 or 7
- High fever goes away with advent of rash
- Note that rubeola as in standard measles is a systemic infection by a paramyxovirus of the Morbillivirus genus
- Recall: Rubeola (paramyxovirus of morbillivirus virdae) -> Standard Measels, Rubella (rubella virus) -> German Measles, Roseola (herpes virus 6 / 7) -> Roseola infantum
- Roseola infantum has a 5-15 day incubation period
- One of the widest ranges of the childhood exanthem-causing systemic infections
- Roseola infantum is marked by high fever in an otherwise well child
- Recall that varicella can also present with fever but will have other non-well symptoms like headaches, photophobia, and conjunctivitis.
- Roseola infantum (not simply "roseola") presents with a pale-pink macular rash as the fever fades.
- Note that, like varicella, roseola's rash can manifest on the hands.
- Roseola infantum's rash can also develop on the tongue or on the mucosal membrane.
- Note that roseola infantum has the palest rash.
[edit] Hand-Foot-and-Mouth Disease
- Hand-Foot-and-Mouth disease is a systemic infection by Coxsackie virus A16 or Enterovirus 71
- HFM has the very short incubation period: 3-6 days.
- Only scarlet fever has a shorter incubation period.
- HFM occurs in 3-year cycles; manifests in summer and fall
- Lesions of coxsackie / enterovirus hand-foo-and-mouth disease are primarily found on the mouth--less so on the hands and feet.
- Note that HFM mouth lesions are easily differentiated from koplik spots of measles (rubeola).
- Hand-foot-and-mouth infections last about 7-10 days
EWWWWWWWWWWWWWWWWWWWWWWWWWWWW nick.co.uk/thelorax
[edit] Scarlet Fever
- Scarlet fever is a systemic distribution of streptococcal toxin
- Fine little discrete papules that are all over the trunk
- Desquamation can be pretty severe: peeling of skin on hands, trunk
- Severe form can even make nails look like they will come off
- Scarlet fever has the shortest incubation period of the exanthems (we studied): 2-4 days.
- Scarlet fever presents as fever, pharyngitis, and a strawberry tongue.
- The rash of scarlet fever begins on the neck and spreads to the trunk and then the extremities.
- Scarlet fever rash is marked by its sandpaper texture.
- There is significant desquamation after resolution of scarlet fever rash.