Female reproductive physiology
From Iusmphysiology
Revision as of 01:11, 8 April 2011 by 24.15.60.132 (Talk)
- started here on 04/07/11.
Female reproductive physiology
Objectives
- Know key characteristics of the H-P-O Axis
- Recognize the structure and functions of female reproductive organs
- Understand Oocyte Mitosis and Meiosis
- Understand Folliculogenesis, Steroidogenesis, Ovulation
- Know key aspects of the menstrual cycle
- Recognize abnormalities of female reproduction
HPO axis
- The HPO axis is the hypothalamus-pituitary-ovary axis.
- Recall that the hypothalamus releases GnRH which stimulates gonadotropes of the anterior pituitary to release LH / FSH which stimulate the ovaries to secrete estrogen and progesterone.
- Pituitary release of LH and FSH can be tonic (consistent at one level) or come in surges.
- Hormone release along the HPO axis is cyclic and highly synchronized.
- Feedback mechanisms of the female HPO axis differ from those of the HPT axis of men.
- While androgens negatively feed back on the hypothalamus, progesterone and estrogen can positively or negatively feed back on hypothalamic GnRH release depending on the amount produced.
- Also, unlike the LH / FSH negative feedback on GnRH release in males, in females, LH / FSH do not negatively feed back on GnRH release at the hypothalamus.
Characteristics of female fertility
- Female fertility has several dogmatic characteristics:
- There is a finite period of fertility in women, namely menarche to menopause.
- Reproductive capacity is intermittent meaning that there are cycles in which reproduction can and cannot occur.
- Note that the reproductive cycle is easily disrupted.
- Germ cells decrease over time; that is, germ cells are not continuously generated as in males and thus decrease in number over time.
- One ova is released at a time.
Determinants of menarche onset
- Menarche is the beginning of the ovulatory cycle and marks the beginning of fertility.
- The commencement of menarche is determined by genetic, nutritional, and environmental factors.
- Timing of menarche have been shown to be strongly correlated among familes.
- Obesity has been shown to accelerate the onset of menarche.
- Family composition and history of abuse have been shown to affect menarche.
***More females in the family is associated with earlier menarche. ***Abuse induces earlier menarche.
Female reproductive organs
- There are two major compartments of female reproductive organs: the ovaries and the ductal system.
- The ovaries are responsible for germ cell maturation and steroidogenesis.
- The ducts are responsible for transporting the ova (unfertilized female gamete) and maintaining the conceptus throughout the pregnancy.
- Ova = ovum: "ovum - the female reproductive cell; the female gamete" per Princeton's wordnetweb
- Conceptus: "embryo: an animal organism in the early stages of growth and differentiation that in higher forms merge into fetal stages but in lower forms terminate in commencement of larval life" per Princeton's wordnetweb
Ovarian structure
- The ovaries are the germ cell incubators in the female GU tract.
- Much like the testes, the ovaries are encapsulated by the tunica albuginea (alb: white).
- The ovary has two compartments: inner and outer medulla.
- The outer medulla contains multiple follicles at subsequent stages of development.
- Ovar reside within the follicles.
- The inner medulla contains interstitial and connective tissues.
Ovarian anatomy
- Recall that the ovary is attached to the posteriolateral wall of the abdomen by the ovarian ligament.
- Through the ovarian ligament travel the ovarian blood vessels to supply the ovaries.
- Recall that the parenchyma and the stroma are opposites: functional tissue of the organ versus structural tissue of the organ.
- Stroma: "the supporting tissue of an organ (as opposed to parenchyma)" per Princeton's wordnetweb
- Note that stroma cells produce androgens.
- The ovary ovulates (releases a mature ova) near the fimbria of the ovarian duct.
- The ovarian duct is made up of the ampulla and the isthmus.
- The isthmus of the ovarian duct receives the ova from the ampulla and shuttle it through the uterine wall to corpus of the uterus.
- Recall that the uterus is composed of the fundus, the corpus (body), and the cervix (neck).
- Recall that the uterus is held in place by the broad ligament of the abdomen.
- The uterus is composed of two layers: the endometrium and the myometrium; the myometrium provides the muscle of contraction.
- The ductal system to carry the ova continues through the corpus of the uterus, through the internal and external os, through the cervix (passed the two fornices), and through the vagina.
Primary hormones produced by the ovary
- Recall that the ovary is responsible for germ cell maturation and steroidogenesis.
- The ovary produces estrogen, progesterone, inhibin, and activin.
- Estrogen is made by the follicles.
- Follicles contain the ova and mature / degenerate as they travel up and down the ovary.
- Progesterone is produced by the corpus luteum.
- The corpus luteum is the degenerating follicle.
- Inhibin negatively feeds back on the anterior pituitary (and not the hypothalamus).
- Estrogen is made by the follicles.
Ovarian steroidogenesis
- The primary hormonal product of the ovaries is estradiol.
- The production of hormones in the ovary requires two cell types and two hormonal signals:
- Theca cells are signaled by LH to produce testosterone.
- Granulosa cells are signaled by FSH to convert testosterone into estradiol (E2) via aromatase.
- Recall that aromatase converts testosterone to E2.
- Granulosa cells:
- Granulosa cells are the only cells of the ovary to express the FSH receptor.
- FSH can induce expression of its own receptor!
- Granulosa cells lack Cyp17, so they cannot generate androgens on their own.
- Recall that Cyp17 is required to convert cholesterol to androgens.
- That is granulosa cells depend on theca cells as a source of androgens.
- Granulosa cells do begin to express the LH receptor as the follicle matures.
- This makes sense as it will undergo luteinization after ovulation.
- Theca cells:
- Recall that theca cells are signaled via LH to produce testosterone.
- Theca cells use cholesterol from the blood and Cyp17 to provide testosterone to the granulosa cells.
- Recall that theca cell are on the outside of the follicle--nice, easy access to blood and cholesterol.
- Theca cells produce primarily androstendione.
- Androgens have pro-aromatase activity at low levels and pro-atresia activity at high levels.
- Stroma cells:
- Stroma cells of the follicle are primarily structural connective tissue.
- However, stromal cells can produce some androgens.
Oocyte development
- As with spermatogenesis, a germ cell precursor yields a series of intermediate cells and finally a mature gamete.
- Recall that the testes are the home of germ cell maturation in males; similarly, the ovary is the site of germ cell maturation in females.
- Also as with males, the germ cell uses a series of mitosis and meiosis to generate mature gametes.
- Cells: oogonia -> primary oocyte -> secondary oocyte (ovum).
- Divisions: mitosis -> meiosis 1 (arrested in phrophase of meiosis 1) -> meiosis 2 (arrested in metaphase of meiosis 2).
- From the top:
- Oogonia (primordial germ cells) originate at the yolk sac and migrate to the genital ridges.
- Note that this step would be the same in males but the genital ridges would become testes, not ovaries.
- Oogonia undergo mitosis to increase in number during the first two trimesters.
- Oogonia mature into primary oocytes; note that this maturation process does not generate new cells.
- Primary oocytes arrest in prophase of meiosis 1.
- Recall that in prophase of meiosis 1, the primary oocyte has made a copy of the genome (and so is 4N), sister chromatids are attached by their centromeres, homologous chromosomes have crossed over, and the centrosomes are moved to the poles.
- Primary oocytes remain in this state until the onset of regular menstruation cycles.
- Note that this is a long period of time during which oocytes are exposed to toxins which can result in chromosomal defects.
- Upon LH spike, primary oocytes progress to secondary oocytes.
- Completing the first division of meiosis (that is, completing meiosis 1, a mitotic like event) generates the first polar body.
- LH spices during menarche and at each subsequent ovarian cycle (period).
- Secondary oocytes are arrested in the metaphase of meiosis 2.
- Recall that in metaphase of meiosis 2, the secondary oocyte has gone through one division (and so is 2N), sister chromatids are attached by their centromeres, and centrosomes have attached spindles to the kinetochores.
- Metaphase of meiosis 2 is also called the ovulatory stage.
- Secondary oocytes remain in metaphase of meiosis 2 until sperm penetrate the cell.
- Sperm penetrate the secondary oocyte, inducing completion of meiosis.
- Completion of the second cell division (that is, completing meiosis 2) generates the 'second polar body.
- Oogonia (primordial germ cells) originate at the yolk sac and migrate to the genital ridges.
- Oocyte count along lifetime:
- Week 20 of gestation: 6 million
- Week 40 of gestation: 2 million
- Menarche: 500K
- Menopaue: 0
The mature follicle
- The mature follicle has 7 layers and 1 space:
- The layers from outside to inside: theca externa, theca interna, basement membrane, granulosa cells, corona radiata (around most of the oocyte), cumulus oophorus (connecting the oocyte with the granulosa cell layer), and the zona pellucida.
- The antrum is a space filled with follicular fluid between the granulosa cells and the corona radiata layer.

- Theca interna / externa.
- The thecal cells of the theca externa and theca interna are signaled by LH to produce androgens that affect the granulosa layer.
- Theca cells have ready access to choleterol from the blood stream (they are on the outside where it is easier to get stuff from the blood).
- Theca cells primarily produce androstendione.
- Androgens have different effects at different levels: high -> follicular atresia, low -> increased aromatase (testosterone -> E2) activity.
- Basement membrane
- The basement membrane holds the follicle together until just before ovulation when the basement membrane disintegrates.
- Granulosa
- Granulosa cells of the granulosa layer are responsible for generating follicular fluid and converting androgens to E2.
- Granulosa cells have an FSH receptor through which they are siganled to convert androgens to E2 (via aromatase).
- Recall that theca cells generate androgens upon LH signaling; it is from theca cells that granulosa cells receive their supply of androgens.
- FSH induces expression of its own receptor in the granulosa cells.
- As the follicle matures, FSH and E2 induce expression of the LH receptor in granulosa cells.
- It makes sense that the LH receptor should begin to be expressed in the granulosa cell because just before ovulation, the granulosa cells will leutinize to become vascular, lipid-rich luteal cells.
- Antrum
- The antrum is filled with follicular fluid produced by granulosa cells.
- Follicular fluid contains FSH, hormones, growth factors, opioids peptides, and plasminogen activators.
Folliculogenesis
- Follicle progression follows a series of maturation (folliculogenesis) steps up one side of the ovary and then goes through ovulation (releases a mature ova).
- Maturation: primordial follicle -> primary follicle -> secondary follicle -> tertiary follicle -> Graafian follicle.
- There are particular characteristics associated with each follicle state:
- primordial follicles have a primary oocyte and a single layer of granular cells.
- primary follicles have a larger oocyte, the first appearance of the zona pellucida, and a layer of granular cells.
- secondary follicles have an oocyte, zona pellucida, multiple layers of granulosa cells, and the first appearance of theca cells.
- tertiary follicles have an oocyte, zona pellucida, multiple layers of granulosa cells, appearance of the antrum, and distinction of the theca interna and externa.
- Graafian follicles have an oocyte, zona pellucida, appearance of the cumulus oophorus, appearance of the corona radiata, multiple layers of granulosa cells, antrum, theca interna, and theca externa.

Role of FSH in folliculogenesis
- Recall that granulosa cells have FSH receptors and are a significant layer of the follicle.
- Recall that the granulosa cells have serve to produce E2 and follicular fluid.
- Recall that follicular fluid is rich in FSH.
- FSH signaling on the granulosa cells causes:
- Increased E2 production (from androgens from theca cells),
- Granulosa proliferation.
- Granulosa proliferation increases the follicle's capacity to produce E2, to generate fluid, and to bind FSH.
Regulation of folliculogenesis
- Recall that the primordial follicle first progresses to the primary follicle stage.
- Movement from the primary follicle to the primary follicle is gonadotroprin-independent.
- That is, consistently throughout life and without the need for gonadotropins primordial follicles are progressing to primary follicles.
Even before puberty?
- Progression from a primary follicle to secondary follicle and beyond is gonadotropin-dependent.
- In most cases, only one follicle per ovarian cycle will progress to secondary follicular stage.
- Note that follicles that progress past the primary follicle stage are committed.
Ovulation
- During ovulation, one of the developing follicles becomes predominant and will rapidly mature and eject its ova to the fimbria.
- The general steps in ovulation include establishing the dominant follicle, atresia of other follicles, LH spike to prepare the microenvironment, acute pre-ovulation changes, and ejection of the ova.
- The dominant follicle is usually established by 5-7 days into the ovarian cycle and will undergo exponential growth.
- As the dominant follicle grows, granulosa cells proliferate and consequently follicular androgen and E2 levels rise.
- As E2 levels rise there is increased feedback on the pituitary, decreased FSH, and therefore decreased gonadotropic effect to help the non-dominant follicles develop.
- Because of these decreased levels of FSH, the non-dominant follicles undergo atresia.
- Non-dominant follicles are generally pre-antrum (that is, secondary follicles or even less mature).
- Upon LH spike, the dominant follicle undergoes a series of changes that prepares it for release of the ova and prepares the microenvironment for fertilization:
- Meiosis reinitiates (moving form prophase of meiosis 1 to metaphase of meiosis 2).
- Steroid production switches from E2 to progesterone.
- This change to production of progesterone is associated with an increase in basal body temperature.
- Blood flow is increased.
What is the scope of this statement? Follicle blood flow, ovarian, uterine?
- Proteolytic enzymes are activated in the follicle.
- 30-36 hours after LH spike the follicle ruptures and ovulation occurs.
- Just before ovulation, the follicle undergoes a series of changes that lead to ovulation:
- Disintegration of the basement membrane,
- Granulosa cells luteinize to become vascular, lipid-rich cells,
- Plasmin cuts up the follicular wall allowing the follicle to enlarge and bulge out from the ovary surface,
- Finally the oocyte is extruded.
Signs of ovulation
- Signs of ovulation can be understood by examining the changes in hormone levels throughout the process:
- Recall that LH has spike causing an increase in androgens.
- Elevated androgens cause an increased libido.
- Recall that LH has spike causing an increase in androgens.
What about the fact that libido has shown to not be associated with androgens in men?
- Recall that increased androgens get converted to an increase in estradiol.
- Elevated estradiol causes increased spinnbarkeit: "the capacity of a viscous liquid (especially the cervical mucus) to be drawn out into a strand or blown up into a bubble" per Princeton's wordnetweb
- Elevated estradiol causes ferning of cervical mucus: ferning occurs in vivo and helps guide sperm through the cervix per wikipedia
- Recall that steroidogenesis switches from E2 to progesterone.
- Progesterone causes an increase in basal body temperature.
- Recall that increased androgens get converted to an increase in estradiol.

Follicular fate
- The follicle has two possible fates: atresia or develop into a corpus luteum.
- Most follicles will undergo atresia.
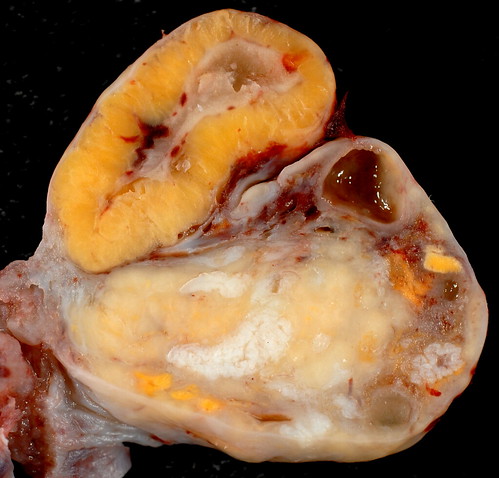
- Corpus luteum formation:
- The corpus luteum is a temporary endocrine structure that develops from a follicle that has evicted its ova.
- Formation of the corpus luteum follows a series of stages like follicular maturity: follicle -> (ovulation) -> early corpus luteum -> mature corpus luteum -> corpus albicans.
- The process of converting a follicle into a corpus luteum is called luteinization.
- Note that lute means "yellow" in Greek and / or Latin.
- So luteinization is a yellowing process.
- In fact, in real life, a fresh corpus luteum is actually yellow.
- The corpus luteum eventually becomes a fibrous structure called the corpus albicans.

Corpus luteum characteristics
- Recall that the corpus luteum is the post-ovulation continuum of the follicle.
- The corpus luteum is comprised of three cell types: theca cells, stroma cells, and luteal cells (from luteinization of granulosa cells).
- Recall that theca cell generate androgens upon LH signaling.
- Recall that stroma cells can generate some androgens.
- Recall that granulosa cells converted androgens to estrogens and then switched to production of progesterone during ovulation.
- Luteal cells produce both estrogen and progesterone.
- The corpus luteum is the primary source of circulating steroids after ovulation.
- Progesterone levels peak 6-8 days after the LH surge.
- The corpus luteum degenerates after 9-11 days.
Mentrual cycle
- Menstruation occurs every 28 days, approximately.
- Menstruation occurs as a withdrawal reaction as the hormone levels decrease as the corpus luteum degenerates and stops producing high levels of androgens, estrogens, and progesterone.
- Menstruation can be described as a cycle of changes occurring at two locations: the ovaries (the ovarian cycle) and the uterus (the uterine cycle).
- There are three distinct phases to the ovarian cycle of menstruation: follicular phase, luteal phase, and menses.
- The follicular phase is composed of follicle maturation.
- The follicular phase can be variable in duration.
- During the follicular phase estrogen levels are elevated (recall that androgens are high and granulosa cells are proliferating).
- As estrogen peaks it has a positive feedback effect on the pituitary causing a spike of LH release.
- There is also a small spike of pituitary FSH release.
- LH surge causes a depression of E2.
- Subsequently, the spike of LH causes ovulation.
- The luteal phase begins at ovulation and ends at menses.
- During the luteal phase hormones rise as the corpus luteum matures, then fall as the corpus luteum degrades.
- The luteal phase is consistently 14 days in duration.
- The menses phase consists of shedding the uterine lining.
- During menses, sex hormone levels are low (the corpus luteum has just finished degrading) and FSH is elevated.
- The phases of the menstrual cycle can also be described by the changes to the uterus (the reproductive tract).
- The uterine cycle of menstruation: the proliferative stage, secretory stage, ischemic stage, and menstrual stage.
- The proliferate stage is characterized by endometrium hypertrophy and formation of spiral arteries.
- Recall that the uterine prolierative stage occurs during the ovarian follicular phase.
- So as the ovary is maturing its follicle, the uterus is regenerating it's surface (where the egg will implant) and increasing vascular access to the surface.
- The secretory stage is characterized by coiling of glands, secretion of mucus, tortuous arteries, and peak thickness of the endometrium.
- Recall that the uterine secretory stage occurs during the ovarian luteal phase.
- So, as the ovary has shed an ovum and is now increasing hormone production via the corpus luteum, the uterus is using glands and arteries of the uterus to modify the uterine microenvironment to the optimal conditions for egg implantation.
- The ischemic stage is characterized by arterial constriction, decreased blood flow, and increased prostaglandins.
- Recall that the ischemic stage occurs during the ovarian menses phase.
- So as the ovary has reached its lowest levels of hormone production, the uterus is decreasing nutrition to the endometrium and allowing the mucosa to undergo necrosis by ischemia.
- The menstrual stage is characterized by desquamation of the endometrium.
- Recall that the menstrual stage occurs during the ovarian menses phase.
- So as the ovary has reached its lowest levels of hormone production, the uterus is shedding its endometrium.
Menopause
- Menopause occurs when no more eggs are available and follicular maturation no longer occurs.
- The average age to run out of eggs (menopause) is 52.
- Menopause is a phenomenon unique to humans.
- Once a patient has run out of eggs, there is less estrogen produced (recall that granulosa cells are the primary source of estrogen and they are found in the developing follicles).
- Less estrogen production means less negative feedback on the anterior pituitary and therefore gonadotropin (LH / FSH) levels are elevated.
- Decreased estrogen also results in hot flashes, decreased bone mass, increased cardiovascular risk, and atrophy of the vaginal epithelium.
- Recall that estrogen inhibits bone mass loss and thus we sometimes supplement at-risk women to prevent osteoporosis.
- Stromal cells of the ovary continue to produce androgens which can be converted to estrone at target tissues.
Abnormalities of female reproduction
Precocious puberty in severe primary hyperthyroidism
- Primary hyperthyroidism is an overactivity of the thyroid that can affect the gonads when TSH cross-reacts with the FSH receptor on granulosa cells.
- When TSH levels are aberrantly high (because of a thyroid defect), TSH will signal development of the gonads through the FSH receptor on granulosa cells of the ovaries or the Sertoli cells of the testes.
- TSH-FSHr signaling causes testicular enlargement in boys and breast development and vaginal bleeding in girls.
- It makes sense that TSH-FSHr signaling in girls causes breast development because we know estrogen is what causes breast development and we know that granulosa cells convert androgen to estrogen.
Is this hypothyroidism or hyperthyroidism?
- Patients with primary hypothyroidism will also show the classic signs of hypothyroidism and can be successfully treated with thyroid hormone replacement.
- Recall that S&S of hypothyroidism: Weight gain, Goiter, Puffy appearance, Loss of hair, Low BMR, low body temp, decreased perspiration, Lethargy, depression, intolerance to cold
Pseudoprecocious puberty versus true precocious puberty
- Recall that pseudoprecocious puberty is gonadotropin-independent; that is, a non-HPG axis source of sex steroids (i.e. androgens or estrogens) has caused secondary sexual development (but will not have caused development of the gonads which require LH and FSH for development).
- Patients with pseudoprecocious puberty show pre-puberty levels of LH but manifest secondary sexual characteristics and early growth arrest.
Primary amenorrhea
- Primary amenorrhea means that menarche has not occurred.
- Primary amenorrhea can be the result of normal variation, a defect at the hypothalamus or pituitary, a defect at the ovary, or a disorder of sexual development.
- Normal variation in sexual development is considered primary amenorrhea if menarche has not occurred by age 16 as long as growth and sexual characteristic development are normal.
- Hypothalamic-pituitary defects cause decreased or non-pulsatile release of GnRH / LH / FSH and result in anovulation.
- Gonadal dysgenesis or other ovarian defects can result in anovulation.
- Gonadal dysgenesis results in fibrous "streaks" instead of functional ovaries.
- Turner syndrome is an example of a gonadal dysgenesis.
- Reproductive tract abnormalities account for 1/5th of primary amenorrhea cases.
Turner syndrome
- Turner syndrome is a missing or structurally abnormal X in an otherwise normal XX female.
- Turner syndrome patients have short stature and ovarian failure.
- Though the ovaries of patients with Turner syndrome initially develop normally, they undergo accelerated atresia during gestation.
- The fact that the ovaries develop normally but then degrade indicates that two healthy X chromosomes are required for maintenance of the ovaries.
- Turner syndrome often presents with primary amenorrhea or delayed puberty.
- The gonadotropins are elevated in Turner syndrome patients because there is no negative feedback via ovary-generated sex hormones.
Secondary amenorrhea
- Secondary amenorrhea means menstruation has ceased for over 6 months
- Possible causes of secondary amenorrhea include pregnancy, poly-cystic ovarian syndrome, and endocrine disorders.
- Endocrine disorders that cause secondary amenorrhea include:
- Hypothyroidism, hyperthyroidism
- Recall that TSH can cross-react with FSH receptor and thus cause precocious puberty.
- Hyperprolactinemia
- Non-classic Congenital adrenal hyperplasia
- Elevates androgens to the point of inhibiting LH / FSH production.
- Hypothyroidism, hyperthyroidism
- Polycystic ovary syndrome
- PCOS is the most common reproductive abnormality in women worldwide.
- PCOS results in chronic anovulism and hyperandrogenism.
- PCOS S&S include obesity and hirsutism.
- Note that hirsut means "hairy" in Greek or Latin.
- PCOS is often preceded by low birth weight and premature pubarche.
- Recall that pubarche is the development of pubic hair.
- PCOS generally occurs with many other metabolic problems, too; not the least of which is insulin resistance.
- STromal hyperthecosis is luteinizing of the theca cells and is correlated with circulating insulin levels.
Conclusions
- The HPO axis is complex and cyclic.
- Oocyte meiosis begins in prenatal life and arrests at prophase of meiosis 1 and again at metaphase of meiosis 2.
- Ovarian steroidogenesis requires proper functioning of theca cells and granulosa cells.
- The menstrual cycle is controlled by hormone changes and results in changes to the ovary and to the genital tract.
- Abnormalities of female reproduction can result in primary and secondary amenorrhea.
- stopped here on 04/07/11.
