Urinary 1 and 2
From Iusmhistology
- started here on 03/21/11.
[edit] Urinary 1
- The kidney has one of the most complex 3 dimensional organizations of all the organs of the body.
- We will study the kidney incrementally, beginning with the uriniferous tubule.
- We will study some simpler kidneys that contain only one papillary, called "unipapillary kidneys".
- The functional unit of the kidney is the uriniferous tubule.
- We have 1 million uriniferous tubules.

[edit] Cortex and Medulla
- The kidney has two major regions: the cortex on the outside and the medulla on the inside.
- The pelvis is the sinus area of the kidney that is "sub-medulla" and forms the collecting area for urine before it enters the ureter.
- Urine is produced by lobes which contain a single renal papillum which dumps urine into the pelvis which dumps into the ureter.
- Small mammals often have only one lobe and therefore one renal papillum.
- Humans have multiple lobes and therefore multiple renal papilla.
- In unipapillary kidneys, the uriniferous tubules run all the way from the cortex to the papillum-pelvic border.
- The urine drips off the papilla (papillum) into the pelvis.


[edit] More on macrostructure
- Each uriniferous tubule is situated in one of the many medullary rays and medullary pyramids found in humans.
- The cortical region contains the glomeruli and is called the medullary ray.
- The medullary area contains the vasa recta, the loop of Henle, and the collecting duct.
- Medullary pyramids are separated by renal columns of Bertin.
- The renal pelvis is the area where the ureter begins to form from the sinus of the kidney.

[edit] Uniferous tubule function
- The uriniferous tubule is made up of epithelial cells.
- The tubule is surrounded by two sets of capillaries:
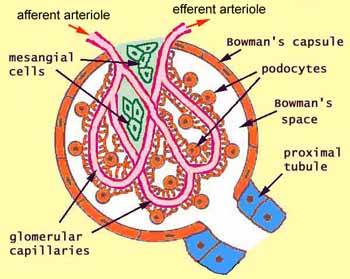
- The glomerular capillaries are within the Bowman's capsule in the cortex.
- The peritubular capillaries are within the medulla, along the length of the loop of Henle and the collecting duct.
- The renal corpuscle is the glomerulus, Bowman's capsule, and the glomerular capillaries.
- The renal corpuscle's function is to filter the plasma passing through the glomerular capillaries.
- The nephron and collecting describes everything other than the renal corpuscle.
- The nephron and collecting duct serve to secrete waste products and reabsorb nutrients to / from the filtrate.
- Note that the kidney filters by throwing out everything and then collecting back the things it wants to keep.
- This is good because the kidney doesn't have to know what needs to be gotten rid of which could be infinite things; the kidney only needs to know what it wants to keep.

[edit] Uriniferous tubule layout and embryonic development
- Though we draw the uriniferous tubule as a simple, linear tract, it is rarely this simple in final 3D form.
- It is important to understand embryonic development to understand why the uriniferous tubule takes its certain and functional 3D form.
- For proper functioning, it is critical that certain sections of the uriniferous tubule lie next to one another.
- The first form of a plasma filtering mechanism in the developing human embryo is called the mesonephric kidneys.
- Mesonephric kidneys reach their maximum size at 8 weeks and then undergo a large change.
- Parts of the mesonephric kidneys persist in men to form:
- the efferent ductules,
- the epididymis,
- the ductus deferens, and
- the ejaculatory duct.
- The cloaca is an early developing orifice that serves to excrete feces and urine.
- The cloaca is common between placental mammals, birds, amphibians, etc.
- The cloaca is retained by birds, amphibians, and reptiles.
- The cloaca in mammals divides and conributes to the anus and the urethra / vagina.
- The early plasma filtering structure is divided into two sections: the mesonephros and the metanephros.
- The metanephros gives rise to the permanent kidneys.
- The metanephros contains the metanephric mesenchyme and the uritic bud.
- The uritic bud and the metanephric mesenchyme are both composed of epithelial cells.
- The uritic bud grows up into the nephrogenic mesoderm which is part of the metanephros.
[edit] Uritic bud and nephrogenic mesoderm interaction
- The uritic bud grows into the nephrogenic mesoderm to form the mature uriniferous tubules.
- The interaction between the uritic bud and the nephrogenic mesoderm is called reciprocal induction.
- Reciprocal induction: "... tissues causing changes in each other due to signals and receptors in each" per this paper
- If the bud doesn't grow up into the nephrogenic mesenchyme, neither tissue becomes what it should.
- Reciprocal induction: "... tissues causing changes in each other due to signals and receptors in each" per this paper
- As the uritic bud grows into the nephrogenic mesenchyme, the uritic bud is the primary epithelial cell tubule structure that will become the collecting duct.
- Recall that mesenchymal cells are connective tissue cells.
- Recall that mesenchyme looks like loose connective tissue with lots of spindly, undifferentiated cells within.
- Renal corpuscles develop along the length of the uritic bud (that is, the developing collecting duct) and therefore can originate from the tip of the uritic bud or from epithelium that develops along side the uritic bud.
- Renal corpuscle and nephron development from the tip of the uritic bud:
- At the tops of the uritic bud, mesenchymal cells of the nephrogenic mesenchyme condense and are induced to make a mesenchymal-epithelial transition (MET).
- Condensation includes proliferation
- These MET cells will become the epithelial cells of the glomerular capsule.
- The bud tip then expands to develop the PCT (proximal convoluted tuble), loop of Henle (LoH), and the DCT (distal convoluted tubule).
- The MET shifted cells of the early glomeruli recruit the formation of blood vessels that will become the glomerular capillaries.
- At the tops of the uritic bud, mesenchymal cells of the nephrogenic mesenchyme condense and are induced to make a mesenchymal-epithelial transition (MET).
- Renal corpuscle and nephron development adjacent to the uritic bud
- Along side the uritic bud, epithelial tracts form as S-shaped or comma-shaped tubule structures.
- The tops of these se epithelial tracts will become the glomeruli and the length will become the PCT, LoH, and the DCT.
- The s-shaped buds from condensation, proliferation, and MET of mesenchymal cells will form the PCT, LoH, and DCT.


[edit] Renal corpuscle structure
- The renal corpuscle demonstrates the unique development of the uriniferous tubule by the way the podocytes surround the glomerular capillaries.
- Note that podocytes are a type of epithelial cell.
- Capillaries are a type of endothelial cell.
- We call the glomerulus the glomerular tuft before fully developed.
- Within the capillaries as they develop within the glomerular tuft, there is connective tissue holding the capillaries in place.
- This connective tissue is called mesangium.
- Bowman's space is the epithelial tract that surrounds the tuft of capillaries.
- Bowmans capsule is made of simple squamous epithelium.
- Note that this place forms a complex structure surrounding the many, convoluted, cross-connected capillaries within.
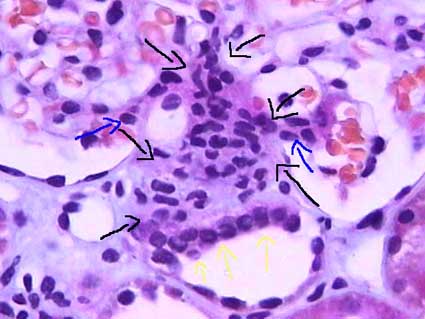
- There are many cell types and structures of the renal corpuscle; each cell type has a specific location and function.
- The afferent arteriole is made of endothelial cells and brings blood to the glomerular capillaries.
- The efferent arteriole is made of endothelial cells and takes blood away from the glomerular capillaries (to the peritubular capillaries).
- The Bowman's capsule is made of epithelial cells and surrounds the glomerular capillaries, forming the Bowman's space beween the Bowman's capsule and the walls of the glomerular capillaries.
- The inside layer of the Bowmans capsule covers the convoluted capillaries and is called the visceral layer; the parietal layer is the outside layer that forms the outer barrier of the glomerulus and is continuous with the epithelium of the PCT.
- The visceral bowmans capsule is made up of podocytes.
- The Bowman's space is the location into which filtrate is first formed by being pressed out of the plasma by hydrostatic forces (primarily, but also including colloid osmotic pressures).
- Often there is pink material in the bowmans space; it is brush border from the proximal tubule that has washed backward during fixation.
- The epithelial cells of the Bowman's capsule are continuous with the epithelial cells that make up the proximal convoluted tubule which carries filtrate.
- The distal convoluted tubule (which is, like the PCT, made up of epithelial cells) passes by the afferent arteriole along side the glomerulus.
- The DCT has specialized cells called 'macula densa cells on the surface that is closest to the afferent arteriole.
- Macula densa cells release signals PGE2 to cause the afferent arteriole to vasodilate and ATP to cause the afferent arteriole to constrict.
- Macula densa cells are more columnar, stain darker, and have rounder nuclei than the endothelail cells of the DCT.
- Juxtaglomerular cells (also called granular cells) are endothelial cells of the afferent arteriole that contain granules of renin.
- Granular cells (AKA juxtaglomerular cells) have a large, flattened nucleus, that is more prominent than the nucleus of lacis (extraglomerular mesangial) cells.
- Granular cells release their renin upon PGE2 binding their EP4 receptor.
- Recall that renin will activate angiotensinogen leading to angiotensin 2 and systemic vasodilation.
- Lacis cells (also called extraglomerular mesangial cells) hold the DCT, the afferent arteriole, and the glomerulus together.
- Extraglomerular mesangial cells may also have some functioning in modifying the signals released by the macula densa cells as they travel to the granular / endothelial cells of the afferent arteriole.
- Lacis cells (extraglomerular mesangial cells) are found between the macula densa cells and the afferent arteriole endothelial cells.
- Lacis cells have a lighter stain and less prominent nucleus as compared to granular (juxtaglomerular) cells.
- This makes sense because granular cells will have granules full of the protein renin.
- Extraglomerular mesangial cells are found between the convoluted capillaries, too, and serve to hold the loops in their structure.
- In this case, the mesangial cells are located within the basement membrane.
- Lacis cells can send processes into the lumen of the capillaries between the endothelial cells.





[edit] Forming a filter at the capillary-Bowman-space junction
- There are three levels of filtration at the capillary-Bowman-space junction.
- The filtrate must first get through the endothelium of the capillary, then through the basement membrane, and then through the feet of podocytes.
- The endothelium of glomerular capillaries is fenestrated without diaphragms to allow only very small proteins and smaller molecules through.
- The basal lamina does restricts even the smallest proteins.
- There are three layers to the basal lamina (basement membrane) of the glomerulus.
- The three layers are probably only separate in slides as a result of processing, but they are still effective markers for pathology.
- The lamina rara extrna is farthest from the lumen of the capillary.
- The lamina rara interna is closest to the lumen of the capillary.
- The lamina densa is between the lamina externa and the lamina interna.
- These layers appear as a light-dark-light pattern in EM.
- Podocytes are a type of epithelial cell that provide the finest level of filtration of the plasma as it crosses into the Bowman space.
- Podocytes project feet that sit on the outside (that is, the Bowman space side) of the capillaries.
- Podocytes often interdigitate to provide a nice tight filter.
- Podocytes form slit pore diaphragms which are very small and let only small molecules through to the bowmans space.
- Water and small molecules pass freely into the Bowman space.
- It is still disputed what factors play the primary role in keeping proteins from entering the filtrate.
- Some say the anionic charge of the basement membrane, which would repel proteins which are generally negatively charged, is the primary factor that hinders protein passage.
- Others point to the podocyte processes and the important proteins that make up the processes (ZO1, nephrin, Neph1) as the primary protein-hindering mechanism.
- Nephrin seems to form a lattice between podocyte processes that would prevent proteins from passing into the bowman space.

- Recall that ZO1 is associated with tight junctions.
[edit] Mesangial cells
- Recall that mesangial cells reside between capillaries within the basement membrane.
- Recall that basement membranes are always made of type 4 collagen!
- Mesangial cells may modulate capillary blood flow.
- Mesangial cells may also act as phagocytes within the basement membrane of the glomerulus.
- Mesangial cells reaches out and cups each capillary around it.
- Mesangial matrix is made up of collagen, glycans, proteoglycans, etc.



[edit] The proximal tubule
- The proximal tubule's primary function is reabsoprtion.
- Approximately 2/3 of the filtrate is reabsorbed in the PT (proximal tubule).
- The proximal tubule is characterized by being large, being eosinophilic (cuboidal, continuous, uniform), and having central nuclei.
- Eosinophilic means the cells will stain very pink.
- The epithelium of the proximal tubule is a simple squamous epithelium.
- The proximal tubule demonstrates cells with brush border and basolateral membrane folding in order to increase its surface area.
- Note that during fixation, the brush border often sloughs off into the lumen.
- The proximal tubule is made up of the proximal convoluted tubule and then then proximal straight tubule' which then proceeds into the descending loop of Henle.
- The proximal straight tubule continues through the outer stripe of the outer medulla.
- "Straight segments ... terminate at a remarkably uniform level ... that establishes the boundary between the inner and outer stripes of the outer ... medulla." per wikipedia
- Note that this is true for both cortical- and juxtamedullar glomeruli-derived proximal straight tubules.
[edit] Cell distinction along the PCT, LoH, and DCT
- Recall that the cells of the PCT, LoH, and DCT are all epithelial cells specialized for reabsorption and / or secretion.
- There are four regions that can be distinguished by cell morphology and characteristic: PCT / thick descending limb, thin descending / thin ascending, thick ascending / DCT, and the collecting duct.
- Note that the thick descending tubule is the same as the proximal straight tubule; the same goes for the distal region: distal straight tubule = thick ascending tubule.
[edit] Cells of the PCT and PST
- Note that the PST = proximal straight tubule = thick descending / proximal loop.
- There are only epithelial cells in the PCT and thick descending loop.
- Epithelium of the PCT is a simple squamous epithelium.
- Recall that the PCT reabsorbs 70% of the filtrate; therefore it makes sense that the cells of the PCT and thick descending tubule are the only cells with a brush border.
- Cells of the PCT and thick descending tubule also have nuclei that are spaced far apart.
- PCT / thick descending tubule epithelial cells stain very pink.
- PCT / thick descending tubule cells are interdigitated.
[edit] Cells of the thin descending and thin ascending tubules
- There are only epithelial cells in the thin descending and ascending tubules.
- Recall that the descending loop is passively, highly permeable to water and solutes.
- Recall that the ascending loop is impermeable to water and actively secretes Na and Cl.
- The epithelial cells of the thin regions are thin cells that stain lightly.
- The nucleus of epithelial cells of the thin tubules is smaller than other nuclei of tubular epithelial cells.
[edit] Cells of the DST and DCT tubules
- Note that the DST = distal straight tubule = thick ascending / distal tubule.
- The epithelium of the DCT and thick ascending tubule is thicker than the PCT and thick descending tubule.
- There are three cell types in the thick ascending and DCT tubules: epithelial cells, macula densa cells, and principal cells.
- Recall that the thick ascending tubule and the DCT are the hormone-responsive regions with many ion transporters to reabsorb Na and Cl in exchange for K.
- The thick ascending tubule is called the "diluting segment" of the nephron because solutes are removed from the filtrate and the epithelium is not very permeable to water, thus making the filtrate more dilute as solutes are reabsorbed and water cannot follow.
- Water at the DST is pretty dilute: 60 mOsm relative to blood's 285 mOsm.
- The DCT is considered part of the LoH.
- Epithelial cells of the thick ascending tubule and DCT need lots of protein to facilitate ion transport and so it makes sense that thick ascending epithelium and DCT epithelium have lots of mitochondria.
- Epithelial cells of the thick ascending tubules and the DCT have apical nuclei that bulge outward (perhaps because of the mt that are pushing them apically).
- Recall that epithelial cells of the DCT will include macula densa cells.
- Macula densa cells appear at the last part of the thick ascending tubule.
- Macula densa cells stain darker than other epithelial cells and are more columnar.
- Macula densa cells are found at the vascular pole of the glomerulus, near the endothelial cells of the afferent arteriole.
- It makes sense that the urinepherous tubule's own DST is near its glomerulus because they started growing at the same time from the same location (recall the MET transition and uritogenic bud).
- The DCT is the first site of intercalated cells.
[edit] Differentiating PST and DST
- Thick descending and thick ascending can be differentiated by their stain and the intracellular location of their nuclei:
- Thick descending epithelium stain darker than thick ascending epithelium.
- Thick descending epithelium has more basally located nuclei while ascending epithelium have apically located nulcei.
- Thick descending has a thicker wall than the thick ascending.
[edit] PCT versus PST and DCT versus DST identification
- Note that PST and PCT can be differentiated because they are never found in the same location: PCT is in the convoluted area and PST is only in the medullary ray area.
- The DST and DCT cannot be differentiated because the DST spans the convoluted area and medullary ray area of the cortex and runs through the outer medulla. The DCT resides only in the cortex.
- Because the DCT and DST are both bound in the cortex, it is likely impossible to tell them apart (unless the structure in question runs right up next to a glomeruli and has macula densa at which point we know it is a DST).


[edit] Differentiationg PCT and DCT
- PCT and DCT can be distinguished by their stain and size:
- PCT epithelium has a brush border but DCT epithelium does not, though often the brush border is not preserved.
- PCT stains darker than DCT, though sometimes it can be the opposite, so good luck with that.
- PCT is made of larger cells than DCT (so with PCT you travel farther around the tubule before finding the next nucleus).

[edit] Cells of the collecting duct
- There are two types of epithelial cells in the collecting duct: principal cells and intercalated cells.
- Recall that the collecting duct's function is to reabsorb water--to concentrate the urine.
- Epithelial cells of the collecting duct are characterized by large, weakly staining (even clear) cells that bulge into the lumen.
- Epithelial cells of the collecting duct have clear distinctions between each cell and have nuclei that do not bulge (like PCT / thick ascending tubule epithelial cells).
- Nuclei are more basal and irregularly shaped.
- Principal cells are hormonally controlled for water reabsorption and are the major site of potassium regulation.
- Principal cells absorb Na and secrete K.
- Principal cells are generally impermeable to water but can become water absorptive when ADH is present (think AQ2).
- Intercalated cells stain darkly, bulge a little into the lumen, have no brush border, have a more apical nucleus than principal cells, and are the site of pH regulation.
- There are three sections to the collecting duct: the connecting tubule and cortical collecting tubule, the outer medullary collecting tubule, and the inner collecting tubule.
- The two proximal sections (connecting duct / cortical collecting duct and the outer medullary collecting duct) have principal and interstitial cells; the inner medullary collecting duct has only principal cells.
- The inner medullary collecting duct is also called the papillary collecting duct.
- The last section of the inner medullary collecting duct is called the duct of Bellini.
[edit] Distinguishing regions of the kidney
- Note that thin segments of the LoH and DCT / PCT never occur in the same area so they can be used to determine the origin of a section.
- Thin loops of Henle are only found in the medulla.
- Recall that the thick proximal tubule terminates at the outer-inner stripe border of the medulla.
- Convoluted tubules are only found in the medulla.
- Thin loops of Henle are only found in the medulla.
- Distinguishing the medulla:
- The inner medulla has only asc / desc thin tubules and the collecting duct.
- The inner stripe of the outer medulla has asc / desc thin tubules, proximal / distal thick tubules, and the collecting duct.
- The outer stripe of the outer medulla has only thick tubules and collecting duct.
- There are no glomeruli in the medulla!
- stopped here on 03/21/11.
- started here on 03/23/11.
[edit] Urinary 2
[edit] Some details from Urinary 1
- Recall that proximal tubule epithelial cells are eosinophilic and have central nuclei.
- Recall that the brush border is usually sloughed off.
- Recall that the proximal tubule has basolateral folds and a brush border to increase the surface area.
- Note the difference between the proximal convoluted tubule and the proximal straight tubule: the straight tubule descends through the outer medullary stripe while the proximal convoluted tubule is confined to the renal cortex.
- Technically the "glomerulus" is the group of capillaries in the capsule.
[edit] Loop of Henle
- Recall that the thin descending loop of Henle is permeable to water and solutes.
- Recall that the thin ascending loop of Henle is impermeable to water and active NaCl reabsorption occurs.
- Recall that the macula densa senses the amount of NaCl in the filtrate.
- When the NaCl level is high, we want slow the filtrate flow rate so we have time to reabsorb all that valuable NaCl; therefore, when the NaCl level in the filtrate is high macula densa cells release ATP to constrict the afferent arteriole and decrease GFR.
- Conversely, very little NaCl in the filtrate at the macula densa means that the filtrate has had lots of time to have its NaCl reabsorbed so we can speed up GFR. In this case, macula densa cells release prostaglandins that cause renin release (and subsequently vasodilation) at the afferent arteriole.
[edit] More kidney superstructure
- Filtrate is dumped into minor calyces which join to form major calicies, which form the renal pelvis, which join to form the pelvic hilum, which is continuous with the ureter.

- Note that the ascending thick tubule is deeper than the descending thick tubule.
- Arcuate vessels follow the boundary of the cortex and medulla, giving off interlobular vessels that give off afferent arterioles and receive stellate vessels.
Do cortical nephrons really not have vasa recta? True! Superficial (cortical) and mid-cortical glomeruli don't have vasa recta. Furthermore, juxtamedullar glomeruli don't have peritubular capillaries. See "Renal vasculature".
- Note that other than the blood vessels that go in and out of the glomerulus (afferent and efferent arterioles), the blood vessels are not specific to a certain nephron (urinepherous tubule); one vessel can service more than one tubule.
- The thick descending tubule = proximal straight tubule = pars recta.
- The human kidney is multilobar and each lobe has a single medulla called "pyramid".
- The cortical tissue of adjacent pyramids (medulla) converge and also, together, run deep toward the renal hilum to form the columns of Bertin.
- Note that renal corpuscles can reside in these columns of Berin but their nephron segment will still reside in one of the neighboring medullary pyramids.
- Collecting ducts empty filtrate into the calyces at the papillary duct.
- Kidney stones (calcification or sedimentation of minerals) can form in the calyces of the kidney.
- We can remove kidney stones through a surgery that pierces the cortex, enters a calyx, and uses a probe to grab / destroy the stone. Percutaneous nephroscopy.
- Kidney stones are painful.
- Stones often form right on the tip of the papilla.
[edit] Renal vasculature
- The order of renal blood flow: renal artery -> interlobar artery -> arcuate artery -> cortical radial artery (imagine these radiating outward from the arc; used to be called interlobular arteries) -> afferent arteriole -> glomerular capillaries -> efferent arteriole.
- The return route can start from two locations:
- Superficial and mid-cortical glomerulus: (from efferent arteriole) peritubular capillaries
- superficial peritubular capillaries return via stellate veins -> arcuate vein...
- deeper peritubular capillaries return via cortical radial vein -> arcuate vein...
- Juxtamedullary glomerulus: (from efferent arteriole) descending vasa recta -> ascending vasa recta -> arcuate vein...
- Superficial and mid-cortical glomerulus: (from efferent arteriole) peritubular capillaries
- Then both follow the same path away from their respective nephron: arcuate vein -> interlobar vein -> renal vein.

[edit] Cortex organization
- A renal lobule is a unit of renal tissue with medullary ray at the center with cortical radial vessels bounding it on the outsides.
- The cortex contains medullary rays, extensions of tubules from the medulla.
- "Under low power the cortex is divisible into alternating bands called the cortical labyrinth, which is recognized by the presence of numerous renal corpuscles and medullary rays, relatively straight collections of epithelial tubules oriented perpendicular to the capsule." per SUNY Downstate Medical
- So medullary rays are the ascending and descending tubules that will run perpendicular to the capsule of the kidney.
- So, a cortical labyrinth is a collection of renal corpuscles with their associated medullary rays.
- Note that in the cortex there is both DCT / PCT (which will run every which way) as well as proximal / distal straight tubules which will run down into the medulla. It is the straight tubules that form medullary rays within cortex cuts.
[edit] Juxtuloglomerular apparatus and the renin-angiotensin pathway
- Renin is released by granular cells (juxtaglomerrular cells).
- Renin cuts angiotensinogen into angiotensin 1 which is cut by angiotenins converting enzyme into angiotensin 2 (at the lungs).
- Angiotensin 2 causes systemic vasodilation.
- At the kidney, angiotensin2-caused vasodilation increases the GFR.
- Juxtaglomerular cells (granular cells) have granules full of renin; the granules can be seen in many slide preparations.
- The apparatus contains the afferent and efferent arterioles, the macula densa, and the extraglomerular cells (lacis cells).
- There are also juxtaglomerular cells which are smooth muscle / endocrine cells.
- Also called "granular cells".
- There are also juxtaglomerular cells which are smooth muscle / endocrine cells.



[edit] Post-kidney urinary ultrastructure
- After the minor, then major calyces and the renal pelvis, filtrate (urine) enters the ureter, then the urinary bladder, then the urethra.
- The calyces, pelvis, ureters, bladder, and uretra all have the same histological structure.
- The only exception is that the walls of the ureters become thicker as they continue.
- The calyces through bladder are transitional epithelium with a lamina propria and smooth muscle.
- The urethra is sometimes transitional epithelium, too, depending on whether male or female.
- Transitional epithelium allows these structures to change volume easily, which is most obviously important in the bladder.
- Note that when no distended the cells look as if they are stacked on top of one another, then they are thin and spread out when distended.
- Transitional epithelium cells are characterized by a bulging apical surface (umbrella cells) and may be bi- or poly- nucleate.
- The lamina propria holds the cells together with connective tissue when changing volume.
- The smooth muscle allows contraction for movement of urine along the tract.
[edit] Transitional epithelium of the bladder
- The transitional epithelium of the bladder has a special mechanism for expanding and contracting its surface area.
- Uroplakins can fold up like a pleat.
- A protein called uroplakin can be moved to the surface or removed from the surface via vesicular movement in order to increase or decrease surface area.
- Vesicles that contain uroplakin are called fusiform cytoplasmic vescicles.
- Uroplakin, as with all membrane proteins, is generated via the rER and golgi apparatus.
- We also know that there is some normal turnover of uroplakin; that is, there is an equilibrium of lysosomal-breakdown and rER-golgi-production.
What is "IC" and "UC" on slide 74.
- Where uroplakin is on the surface, the membrane is thicker; there are thinner areas of membrane that are distict in EM of bladder epithelium.



[edit] Smooth muscle of the bladder
- Smooth muscle of the calyces, pelvis, and ureters are helical in pattern.
- Smooth muscle in the bladder is longitudinal and runs in all directions.
Be able to draw the whole urinipherous tubule and all the regions.
- stopped here on 03/23/11.
