Exam 2 Physical Diagnosis Objectives
From Iusmicm
(Difference between revisions)
| Line 53: | Line 53: | ||
*Not specific to the heart yet the most important. | *Not specific to the heart yet the most important. | ||
*Angina pectoris: pain resulting from an imbalance of myocardia perfusion and myocardial functional demand. | *Angina pectoris: pain resulting from an imbalance of myocardia perfusion and myocardial functional demand. | ||
| + | **Classically presents as the pathognomonic '''Levine's sign''': clutching fist over sternum with flexion at the hips. | ||
{|border="1" | {|border="1" | ||
!Descriptor | !Descriptor | ||
| Line 86: | Line 87: | ||
|Nonspecific | |Nonspecific | ||
|} | |} | ||
| - | * | + | *Common causes of chest pain include: CAD, aortic valvular disease, pulmonary hypertension, mitral valve prolapse, pericarditis, idopathic hypertrophic subaortic stenosis, dissection of the aorta, pulmonary embolism, penumonia, pleuritis, pneumothorax, costochondritis, arthritis, muscular spasm, bone tumor, herpes zoster, ulcer disease, bowel disease, hiatal hernia, pancreatitis, cholecystitis, anxiety, depression. |
| + | |||
| + | =====Palpitations===== | ||
| + | *Palpitations are not necessarily a sign of disease. | ||
| + | *Palpitations are often reported upon the occurrence of "forceful contraction" which result from increased stroke volume. | ||
| + | *Consider: primary cardiovascular issues, thyrotoxicosis, hypoglycemia, fever, anemia, pheochromocytoma, and anxiety. | ||
| + | *Consider: caffeine, tobacco, other drugs | ||
| + | *Common causes: atrial premature beats, nodal premature beats, ventricular premature beats, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation, multifocal atrial tachycardia, ventricular tachycardia, heart block, sinus arrest, bronchodilators, digitalis, antidepressants, smoking, caffeine, thyrotoxicosis | ||
| + | |||
| + | =====Dyspnea===== | ||
| + | *'''Paroxysmal nocturnal dyspnea''' occurs when the pt is supine (usually sleeping at night). | ||
| + | **Supine position increases blood volume in the thorax and therefore the work of the right heart, resulting in heart failure. | ||
| + | **'''Orthopnea''' may be reported: the need to sleep propped up on many pillows. | ||
| + | **Look for pitting edema in the legs as another indicator of heart failure. | ||
| + | *'''Dyspnea on exertion (DOE)''': occurs via pulmonary disease or chronic congestive heart failure | ||
| + | *'''Treponema''': when a pt has less dyspnea when lying on the right or left side. | ||
| + | *General causes of dyspnea include: left ventricular failure, mitral stenosis, obstructive lung disease, asthma, restrictive lung disease, pulmonary embolism, pulmonary hypertension, anxiety, decreased oxygen pressure, and decreased oxygen carrying capacity. | ||
| + | |||
| + | =====Syncope===== | ||
| + | *Syncope is defined as '''loss of consciousness AND loss of postural tone'''. | ||
| + | *Orthostatic hypertension can lead to syncope. | ||
| + | **Micturition syncope occurs in older men (usually) who have to urinate during the night and (because they have just moved from supine to standing) experience syncope. | ||
| + | *Vasovagal syncope occurs because of a '''sudden fall in systemic vascular resistance without a compensatory increase in cardiac output (because of increased vagal--parasympathetic--signal)'''. | ||
| + | **Usually accompanied by ''presyncopous s/s'': pallor, nausea, weakness, blurred vision, light headedness, perspiration, yawning, diaphoresis, hyperventilation, epigastric discomfort (sinking feeling). | ||
| + | *'''Carotid sinus syncope''' occurs because of '''an hypersensitive carotid sinus (or excessive stimulation of the carotid sinus)''' which leads to inappropriate baroreceptor signaling that leads to hypotension and a risk of syncope. | ||
| + | **The reflex can cause bradycardia (slowing the heart rate, decreasing perfusion of the brain, and syncope) or vasodepression (decreased vasoconstriction, decreased perfusion, and syncope). | ||
| + | **'''Post-tussive syncope''' is when coughing increases the thorasic pressure (usually in pts with chronic obstructive disease) and thus activates the carotid sinus reflex and induces syncope. | ||
| + | |||
| + | =====Fatigue===== | ||
| + | *Most common causes of fatigue are anxiety and depression. | ||
| + | *Fatigue has poor specificity for cardiac issues. | ||
| + | |||
| + | =====Dependent Edema===== | ||
| + | *'''Dependent''' edema means that it is '''a function including gravity'''; that is, dependent edema is edema that is affected by gravity. | ||
| + | *Classically, dependent edema is seen in the lower limbs and it best in the morning after having been supine for hours and is worse at the end of the day when the pt has been upright and gravity has moved the fluid to the legs. | ||
| + | *Symmetrical swelling indicates a systemic cardio-pulmonary issue as opposed to an infectious agent. | ||
| + | *'''Cardiac causes of edema are usually preceded by dyspnea.''' | ||
| + | |||
| + | =====Hemoptysis===== | ||
| + | *Hemoptysis is the coughing up of blood. | ||
| + | *Mitral stenosis is an important cuase of hemoptysis. | ||
| + | *More in chapter 13. | ||
| + | |||
| + | =====Cyanosis===== | ||
| + | *'''Differential cyanosis''' is when cyanosis is seen '''only in the lower extrimities'''. | ||
| + | **Differential cyanosis is related to a right-to-left shunt (usually through a patent ductus arteriosus). | ||
| + | **Right-to-left shunt at the ductus arteriosus usually results from pulmonary hypertension. | ||
| + | **Cyanosis occurs only in the lower extremities because blood from the pulmonary artery (deoxygenated) mixes below the carotid / subclavian (which would take the blood to the head / arm). | ||
====Interpret the symptoms of cardiac disease from a clinical scenario==== | ====Interpret the symptoms of cardiac disease from a clinical scenario==== | ||
Revision as of 16:56, 11 November 2011
Chapter 14
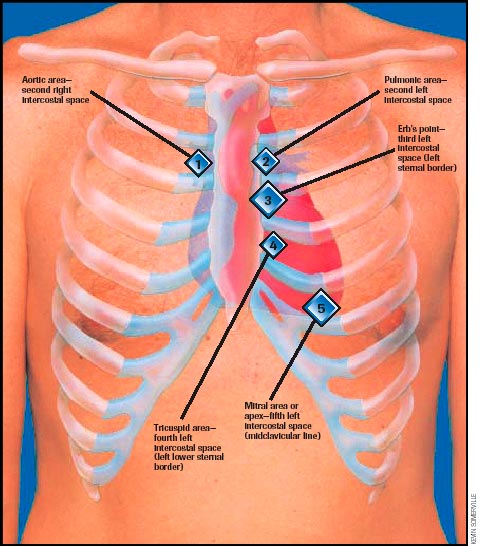
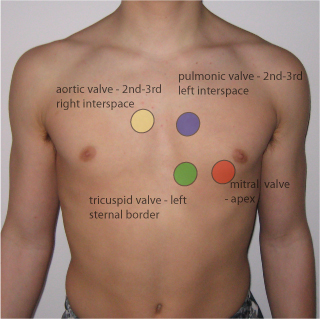
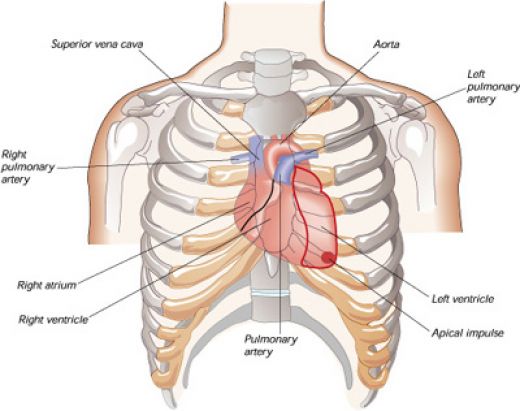
Describe and recognize the surface topography of the heart and utilize that knowledge to describe the physical findings of the heart
Describe and recognize the four classic auscultatory areas and Erb’s point
- The auscultation locations are focused on listening to the valves, though the names of the locations do not necessarily correlate with where the same valve is heard best.
- Aortic: second intercostal space, right sternal border (2ICS-RSB)
- Pulmonic: second intercostal space, left sternal border (2ICS-LSB)
- Tricuspid: left lower sternal border (about the fifth intercostal space; LLSB)
- Mitral: cardiac apex at the fifth intercostal space, mid-clavicular line (5ICS-MCL)
- Erb's point: third intercostal space, left sternal border (3ICS-LSB)
- Location of best pulmonic / aortic valve auscultation

Describe the cardiac cycle and be able to clinically correlate the cycle to a patient’s cardiac exam
- There are four heart sounds: S1, S2, S3, S4
- S1 is the closure of the AV valves: mitrial (left, systemic side) and tricuspid (right, pulmonary side)
- S2 is the closure of the semilunar valves: aortic (left, systemic side) and pulmonary (right, pulmonary side)
- S1 and S2 are normally audible in all individuals.
- S3 and S4 are normal in children and young adults but indicate pathology in adults.
- The presence of S3 or S4 creates a gallop sound and thus they are called gallop sounds.
- S3 occurs at the end of rapid ventricular filling.
- S3--when audible--indicates volume overload.
- Causes of volume overload may include CHF or valve lesions causing regurgitation.
- S3 has a specificity of 90%.
- NB: is is normal to hear S3 in children and youth.
- S4 occurs at the end of diastole.
- S4 can be simulated by speaking the word "middle". S4 is the "ddle" of "middle" where the "mi" is S1 (closing of AV valves).
- NB: S4 is normal in children and young adults.
- S4 in a pt older than 40 is indicative of a noncompliant or stiff ventricle.
- Pressure overload as in CHD is the cause of a noncompliant ventricle.
- Physiologic split of S2 with accompanied sinus arrythmia:
- S2 is often split, especially upon inspiration.
- During inspiration, the intrathoracic pressure is lower causing more blood from the SVC and IVC to enter the right atrium / ventricle.
- Increased right heart filling results in a longer duration of systole and therefore a later closure of the pulmonic valve.
- Thus P2 (the pulmonic component of S2--that is, the closing of the pulmonic valve) occurs later than A2 (the aortic component of S2--that is, the closing of the aortic valve).
- Initially, the return of blood from the pulmonic bed to the left heart will be relatively decreased so the left heart reflex induces sinus arrythmia.
- Sinus arrythmia is an increased heart rate after respiration and is a misnomer because it is not a true arrythmia.
- http://howmed.net/wp-content/uploads/2010/09/cardiac-cycle.bmp


Recognize the main symptoms of cardiac disease and how these symptoms can identify disease
- The main symptoms of cardiac disease are: chest pain, palpitations, dyspnea, syncope, fatigue, dependent edema, hemoptysis, and cyanosis.
Chest pain
- Not specific to the heart yet the most important.
- Angina pectoris: pain resulting from an imbalance of myocardia perfusion and myocardial functional demand.
- Classically presents as the pathognomonic Levine's sign: clutching fist over sternum with flexion at the hips.
| Descriptor | Angina | Non Angina |
|---|---|---|
| Location | Retrosternal, diffuse | Left inframammary, localized |
| Radiation | Left arm, jaw, back | Right arm |
| Character | Aching, dull, pressing, squeezing, viselike | Sharp, shooting, cutting |
| Intensity | Mild, severe | Excruciating |
| Duration | Minutes | Seconds, hours, days |
| Precipitation | Effort, emotion, eating, cold | Respiration, posture, motion |
| Relief | Rest, Nitroglycerin | Nonspecific |
- Common causes of chest pain include: CAD, aortic valvular disease, pulmonary hypertension, mitral valve prolapse, pericarditis, idopathic hypertrophic subaortic stenosis, dissection of the aorta, pulmonary embolism, penumonia, pleuritis, pneumothorax, costochondritis, arthritis, muscular spasm, bone tumor, herpes zoster, ulcer disease, bowel disease, hiatal hernia, pancreatitis, cholecystitis, anxiety, depression.
Palpitations
- Palpitations are not necessarily a sign of disease.
- Palpitations are often reported upon the occurrence of "forceful contraction" which result from increased stroke volume.
- Consider: primary cardiovascular issues, thyrotoxicosis, hypoglycemia, fever, anemia, pheochromocytoma, and anxiety.
- Consider: caffeine, tobacco, other drugs
- Common causes: atrial premature beats, nodal premature beats, ventricular premature beats, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation, multifocal atrial tachycardia, ventricular tachycardia, heart block, sinus arrest, bronchodilators, digitalis, antidepressants, smoking, caffeine, thyrotoxicosis
Dyspnea
- Paroxysmal nocturnal dyspnea occurs when the pt is supine (usually sleeping at night).
- Supine position increases blood volume in the thorax and therefore the work of the right heart, resulting in heart failure.
- Orthopnea may be reported: the need to sleep propped up on many pillows.
- Look for pitting edema in the legs as another indicator of heart failure.
- Dyspnea on exertion (DOE): occurs via pulmonary disease or chronic congestive heart failure
- Treponema: when a pt has less dyspnea when lying on the right or left side.
- General causes of dyspnea include: left ventricular failure, mitral stenosis, obstructive lung disease, asthma, restrictive lung disease, pulmonary embolism, pulmonary hypertension, anxiety, decreased oxygen pressure, and decreased oxygen carrying capacity.
Syncope
- Syncope is defined as loss of consciousness AND loss of postural tone.
- Orthostatic hypertension can lead to syncope.
- Micturition syncope occurs in older men (usually) who have to urinate during the night and (because they have just moved from supine to standing) experience syncope.
- Vasovagal syncope occurs because of a sudden fall in systemic vascular resistance without a compensatory increase in cardiac output (because of increased vagal--parasympathetic--signal).
- Usually accompanied by presyncopous s/s: pallor, nausea, weakness, blurred vision, light headedness, perspiration, yawning, diaphoresis, hyperventilation, epigastric discomfort (sinking feeling).
- Carotid sinus syncope occurs because of an hypersensitive carotid sinus (or excessive stimulation of the carotid sinus) which leads to inappropriate baroreceptor signaling that leads to hypotension and a risk of syncope.
- The reflex can cause bradycardia (slowing the heart rate, decreasing perfusion of the brain, and syncope) or vasodepression (decreased vasoconstriction, decreased perfusion, and syncope).
- Post-tussive syncope is when coughing increases the thorasic pressure (usually in pts with chronic obstructive disease) and thus activates the carotid sinus reflex and induces syncope.
Fatigue
- Most common causes of fatigue are anxiety and depression.
- Fatigue has poor specificity for cardiac issues.
Dependent Edema
- Dependent edema means that it is a function including gravity; that is, dependent edema is edema that is affected by gravity.
- Classically, dependent edema is seen in the lower limbs and it best in the morning after having been supine for hours and is worse at the end of the day when the pt has been upright and gravity has moved the fluid to the legs.
- Symmetrical swelling indicates a systemic cardio-pulmonary issue as opposed to an infectious agent.
- Cardiac causes of edema are usually preceded by dyspnea.
Hemoptysis
- Hemoptysis is the coughing up of blood.
- Mitral stenosis is an important cuase of hemoptysis.
- More in chapter 13.
Cyanosis
- Differential cyanosis is when cyanosis is seen only in the lower extrimities.
- Differential cyanosis is related to a right-to-left shunt (usually through a patent ductus arteriosus).
- Right-to-left shunt at the ductus arteriosus usually results from pulmonary hypertension.
- Cyanosis occurs only in the lower extremities because blood from the pulmonary artery (deoxygenated) mixes below the carotid / subclavian (which would take the blood to the head / arm).
Interpret the symptoms of cardiac disease from a clinical scenario
Apply the components of the physical exam of the heart to a patient
Clinically correlate the symptoms and physical exam findings pertaining to the heart
Give a diagnosis and/or differential diagnosis based on symptoms and/or physical exam findings of the heart
Describe findings from the history and physical exam in the written history and oral case presentation
Chapter 20
- Describe the joint motions of the following joints: shoulder, knee, wrist, and hand.
- Describe the physical examination of the following joints: shoulder, knee, wrist, and hand.
- Apply the components of the physical examination of the musculoskeletal system to a patient.
- Differentiate diseases based on clinical features for the following joints: hands and wrists, knee, and shoulder.

